Articular cartilage injuries can be life changing events. A person who was once a very active and healthy individual can be forced to adopt lifestyle changes where they have to avoid activities that they once enjoyed (running, skiing, hiking or even walking). This can be a devastating event to an individual and lead to other health consequences such as weight gain and depression.
Articular cartilage is the covering of the bones that creates a smooth and fluid movement of our joints. Injuries to cartilage can lead to defects or potholes of the surface and expose the underlying and painful bone. These injuries ultimately can develop into arthritis which is when the entire joint surface is involved. This results in rough surfaces that do not move smoothly and subsequently cause pain.

Figure 1: The right knee (left in picture) shows bone on bone arthritis with complete loss of cartilage as indicated by loss of space between bones. The left knee (on right) is a normal looking knee.

Figure 2: Picture on left is a arthroscopic photo of normal appearing articular cartilage. Picture on right is a picture of arthritis (wide spread cartilage deterioration).
Once arthritis has set in and involves both sides of joint or there is wide spread deterioration, there are not any restoration options. Usually, this results in the need for a joint replacement with metal and plastic. It is best to put this off as long as possible, as a revision would likely to be required during their lifetime. This is not an optimal situation as having a good outcome with revision joint replacements is not predictable. If it is treated before both sides are involved, the joint can be restored with the placement of either autologous (from you) cartilage cell implantation or an allograft (donor tissue) plug of cartilage and bone. Which procedure is for you involves a complex algorithm. There are many issues to consider when choosing the right procedure.
Matrix Autologous Chondrocyte Implantation
MatrixAutologous chondrocyte implantation (MACI) is a procedure designed to repair a contained cartilage defect in your knee. In order to perform this procedure, a sample of your cartilage is obtained during an arthroscopy. This cartilage is then sent sterilely to a lab in Boston, where they extract the cartilage cells, then grow and replicate them. These cells are then sent to your surgeon, implanted onto a collagen sheet, the day of your MACI procedure and they are implanted into the defect (pot hole) in your knee. This procedure was first done in 1987 in Sweden and since many thousands have been performed. The results of ACI are good and excellent in 75-80% of properly selected patients. A 20% failure rate is higher than we usually like in orthopedic surgery, but the absolute holy grail for cartilage repair is yet to be discovered. MACI presents a great option for patients, whom otherwise, have a very poor prognosis.
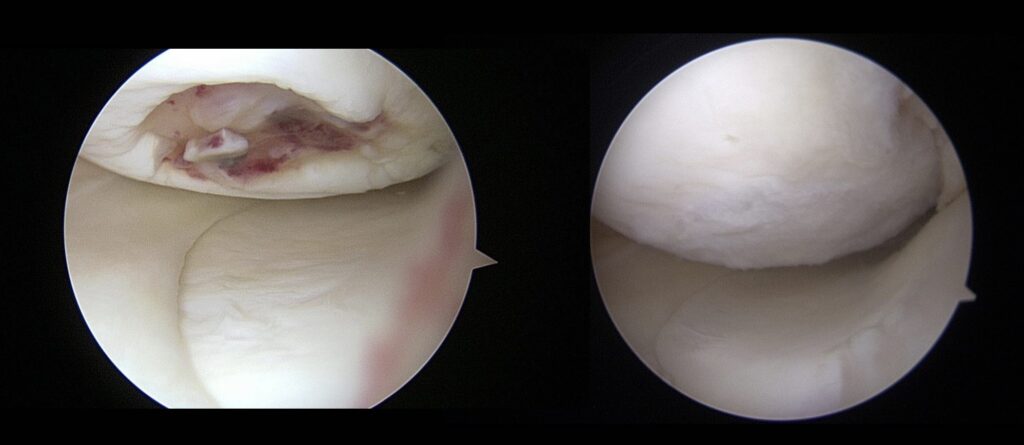
Figure 3: Left picture shows a picture of a cartilage lesion of the medial femoral condyle of the knee. The picture on the right shows the same lesion 15 months after ACI.
While ACI results in very good outcomes in many patients, there is a relatively high rate of return to surgery for various reasons. Most of these re-operations are for debridement of cartilage overgrowth, where the cells simply grow too much cartilage. That was the case for the patient in Figure 3 where the cartilage repair simply had to be smoothed out. Other reasons for return to surgery include development of scar tissue, graft failure, or new injury unrelated to the surgery.
Cartilage preservations experts like myself are very excited about the recent approval of the next generation of cartilage implantation procedures. The initial procedure utilized periosteum as a cover that was stitched with micro-sutures to seal the defect. The second generation utilized a collagen membrane. With these procedures the cells were injected underneath the cover after it was sealed. The cartilage cells dispersed under the membrane and adhered to the bone. Most of the results that are currently are published have utilized one of these techniques (most are actually periosteum which had the highest risk of complication). The cutting edge technique of impregnating the cartilage cells onto a membrane is a very organized fashion. The membrane is simply glued into place. This technique has been utilized for years in Europe and was just approved to be utilized in the United States last month. We are very excited as the early results suggest the outcomes will be better.
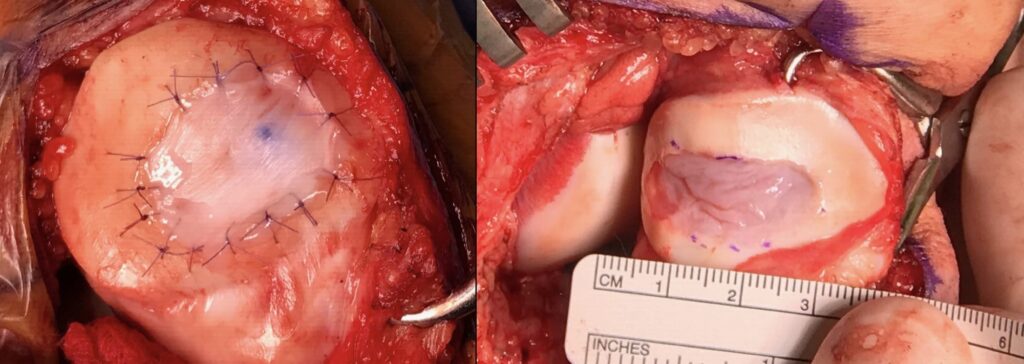
Figure 4: On right, Second generation ACI utilizing a collagen membrane to seal the cartilage cells into the defect. On left, 3rd generation utilizing a membrane impregnated with autologous cartilage cells.
Osteochondral Allograft
There are other surgical and non-surgical techniques to address these injuries. For example, osteochondral allograft (OCA) is where a fresh human donor graft of cartilage and bone is implanted into your knee. This technique also has very good results with 85% survival of graft at 15 years. The negative side of this procedure, is that if it fails, the only subsequent option is a knee replacement or rarely a repeat OCA. If an ACI procedure fails, OCA is typically still an option for your knee. The advantage of OCA is that it can cover very large lesions with higher success rates.
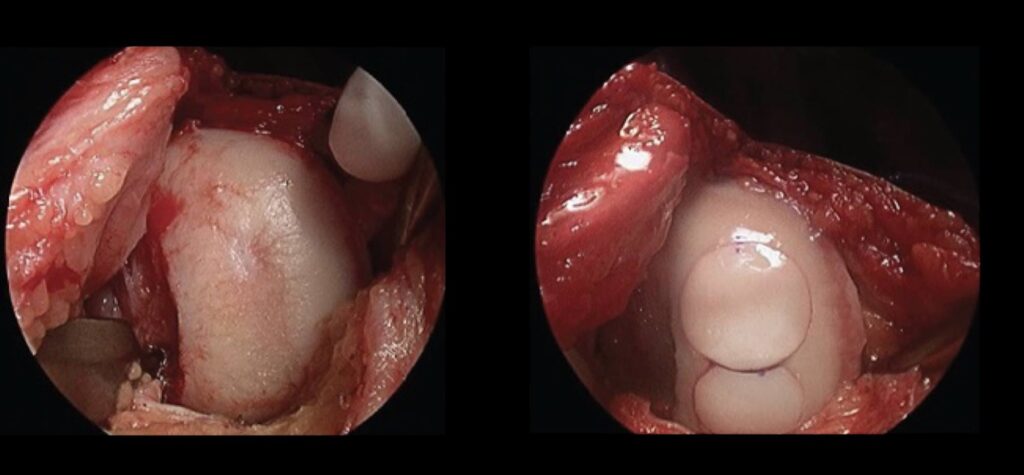
Figure 5: These images demonstrate a medial femoral condyle of a knee before and after Osteochondral Allograft.
Stem Cells and Platelet Rich Plasma (PRP)
Another option for treating patients with cartilage lesions and arthritis involves injecting bone marrow concentrate, PRP or even umbilical tissue into the joint in order to promote cartilage growth and healing. This has the advantage of being non-surgical with extremely low risk of complications. The primary disadvantage for these treatments is that they are still experimental and thus, are not covered by insurance companies. Although, they are still experimental, there is mounting evidence to support their use. For details of these treatments, please see the articles and references posted on my website.
If you would like to know if you are a candidate for one of these procedures, please call my office at (719) 822-6277 and request a consultation.
Chris Jones, MD



