
Anterior Cruciate Ligament (ACL) Tear
Anterior Cruciate Ligament (ACL) Tear
Going to the doctor can be a difficult and emotional experience. This is even more stressful when potential surgery is a consideration. Hopefully the information listed below can alleviate some of the stress and answer any questions that may arise.
Knee Anatomy
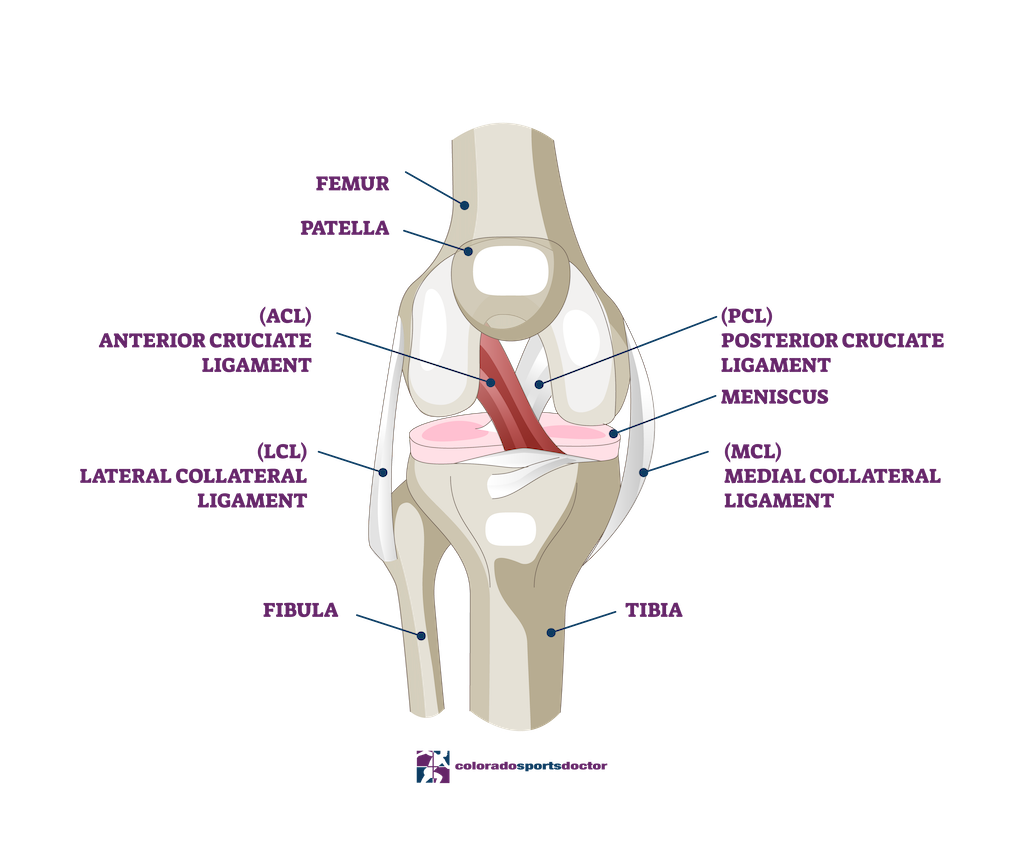
The knee joint is a complex structure composed of bones, ligaments, cartilage, and menisci, all working harmoniously to provide stability and mobility. The primary bones involved are the femur (thigh bone), tibia (shin bone), and patella (kneecap). Ligaments like the Anterior Cruciate Ligament (ACL) connect these bones, ensuring joint stability by limiting excessive movement.
Cartilage, a smooth, white tissue, covers the ends of these bones within the joint, providing a slick surface that allows them to glide over each other smoothly. The knee has two types of cartilage: articular cartilage and meniscal cartilage. The articular cartilage covers the bone ends, while the menisci are crescent-shaped discs between the femur and tibia, acting as shock absorbers and facilitating load distribution throughout the joint.
The knee’s stability is severely compromised when a ligament such as the ACL is torn. The ACL provides crucial stability during side-stepping, running, and cutting motions. Without it, the knee can become unstable and prone to giving way, leading to further damage to the cartilage and menisci and increasing the risk of developing osteoarthritis.
Injuries | ACL Tear
Injury to the ACL is a common issue, especially among athletes and active individuals. This type of injury involves a tear in the ligament, which can occur due to sudden twists, direct impacts, or deceleration movements. As a result, the knee loses its stability, leading to a sensation of instability or episodes where the knee gives way during physical activities.
Aside from the ACL, other structures in the knee can also be damaged during the injury. The articular cartilage may become frayed or eroded, and the menisci tear. Damage to these structures can significantly affect the knee’s function and contribute to chronic pain and degenerative changes within the joint.
Without the ACL, the femur and tibia can slide inappropriately over each other, causing further damage to the existing cartilage and menisci. This condition leads to mechanical issues and increases the risk of early-onset osteoarthritis, where the degeneration of joint structures can severely impact the quality of life.
Treatment
Surgical intervention is typically recommended for individuals with a torn ACL, especially those who are physiologically young and wish to maintain an active lifestyle. ACL tear surgery aims to create a new ligament that restores stability to the knee and prevents further damage to the articular cartilage and menisci.
The procedure involves an arthroscopic-assisted technique where the surgeon uses small incisions to access the knee joint. A graft, taken from the patient’s patellar tendon, hamstring tendons, or donor tissue, creates a new ACL. This graft is securely attached to the bones to restore joint stability. Any damaged cartilage or menisci encountered during surgery are either repaired or debrided to enhance knee function.
Recovery from ACL tear surgery involves a combination of physical rehabilitation and a gradual return to activity. Initially, patients are advised to use crutches and avoid weight-bearing activities. Over time, with guided physical therapy, they regain strength and mobility in the knee. Most patients can return to routine activities within a few months, although full recovery and return to high-demand sports may take several months to a year.
Recovery
Post-operative care for ACL tear surgery focuses on minimizing pain, reducing inflammation, and restoring function. Patients often experience significant pain relief shortly after surgery, especially those who have learned to live with chronic instability and pain. Early movements are encouraged to prevent stiffness and promote blood flow to the healing tissues.
Physical therapy plays a crucial role in recovery. For the first few months, patients typically attend physical therapy sessions multiple times a week. These sessions focus on regaining strength, improving range of motion, and enhancing proprioception (the body’s ability to sense movement and position). Adherence to the rehabilitation protocol is vital for achieving optimal outcomes.
Most patients can return to sedentary jobs within a week, with prolonged standing or walking restrictions. Light-duty work is recommended for several months. As quadriceps strength improves, patients gradually transition from using crutches to walking independently. Those engaged in physically demanding jobs or sports may require extended rehabilitation before fully resuming their activities.
What is wrong with my knees?
When you injured your knee, you tore one of the main ligaments which provides stability to the knee, the anterior cruciate ligament (ACL). Without the ACL, the knee will be unstable and give way if any side stepping, running or cutting motions are attempted. When your knee was injured, you may have damaged some of the cartilage and/or the menisci in the knee as well.
What is a ligament?
A ligament is a cord-like structure that connects two bones together at a joint and allows motion while providing stability. Stability refers to the joint moving in the proper plane while maintaining close apposition of the joint surfaces. When a ligament is torn, stability is compromised and the joint surfaces do not maintain this apposition and the bones can slide inappropriately on one another. This inappropriate motion can cause further damage to the cartilage and menisci.
What is cartilage?
Cartilage is the smooth white material that covers the ends of our bones in the joints. It provides a slick surface and allows the bones to glide over each other.
What are menisci?
Menisci are another form of cartilage that look like bumpers between the bones. Their purpose is to provide cushion between the bones and disperse contact pressures over a greater area.
Recommended ACL tear treatment?
A physiologically young person who wishes to remain active will have a difficult time without a functioning Anterior Cruciate Ligament. The knee will likely be unstable and suffer “giving way” or “buckling” episodes. During these episodes, the femur (thigh bone) and the tibia (leg bone) slide across each other and potentially cause new or further damage to the cartilage and menisci. For this reason, I recommend that you have surgery to correct the problem.
What is the goal of ACL surgery?
The goal of the surgery is to create a new ACL that will prevent the “giving way” or “buckling” episodes, and, hopefully prevent any further damage to the articular cartilage and menisci.
How is the ACL surgery performed?
The ACL cannot be repaired because it is destroyed when it tears. Therefore, I make a new ACL using tissue that I take from somewhere else. This tissue can be from the patellar tendon in the front of your knee, your hamstring tendons, or allograft (donor) tissue.
What if I have persistent buckling episodes and do not have surgery?
Based on current medical knowledge, the likelihood of causing further damage to the knee and subsequently early onset of arthritis is very high.
Can I wear a brace instead of having surgery?
Although brace construction has come a long way, the best brace cannot substitute for a functioning ACL. Studies indicate that braces may prevent instability episodes at low loads(ie. Walking), but at higher physiologic loads (ie. Cutting or pivoting) they cannot.
What is ACL tear surgery like?
The surgery is done via arthroscopic-assisted technique. That means that although all of the work inside your joint is performed through three 1⁄2” incisions, the graft is harvested through an approximately 1 to 3 inch incision.
Will torn cartilage and menisci be taken care of during the surgery?
Yes, torn cartilage and menisci will either be debrided or repaired at the time of the surgery. Menisci are very important to the normal function of your knee so I am very aggressive in attempting to repair them if it is at all possible. If one of your menisci require repair, an additional 2-3inch incision may be necessary on the inside or outside of your knee.
How long will surgery take?
Depending on how much other damage is encountered in your knee, the surgery will take around two hours.
How long will you stay in the hospital?
Patients enter the hospital in the morning, have surgery and go home the same day. This is called outpatient surgery.
How successful is the surgery?
This type of surgery is successful about 90-95%of the time. No operation is 100% successful in every patient, but the procedures we perform are reliable and will help restore your knee’s function. The success of your operation depends on many factors including:
- The amount of damage to the other structures in the knee
- Your body’s response to the injury and surgery
- Your compliance with post-operative rehabilitation
What are the potential complications of surgery?
Surgery is a complex and delicate process designed to repair damage structures deep within the human body. Complications can occur, but fortunately are rare. Infection can occur (<1%) and may require antibiotics and surgery to clean out the joint. Injury to peripheral nerves can also occur but are also uncommon (<1%). Most often the injury is a stretch injury due to manipulation of the extremity during surgery or compression by the tourniquet. These are usually temporary and resolve by 2-6 weeks. Permanent injury can occur but is exceedingly rare. A small nerve that supplies sensation to the outside part of the leg just below the knee is almost always sacrificed during the graft harvesting. This may leave you with a small area of “numbness” on the front of your leg.
When can I return to routine activities of daily living?
As soon as you are comfortable, I encourage you to be up and moving around. By the first or second post-operative day, I expect that you will move easily around your house with crutches and possible venture outdoors. As soon as you have recovered adequete quadriceps strength to support your weight without difficulty, I would like you to discard the crutches. There are particular circumstances where you will require a brace for a period of time, and I will let you know if that is the case.
When can I return to work?
For most sedentery jobs, I recommend a week off work. When you return to work your knee will be sore but you should be able to manage as long as you do no prolonged standing or walking. You will be on “light-duty” for 4 to 6 months depending on your work demands. These are merely guidelines and may need to be altered based on your individual recovery.
How is my knee rehabilitated?
You can perform many of the necessary exercises by yourself at home. However, I ask that you work very closely with the physical therapist and plan on going to therapy 2-3 times per week for at least the first 2 or 3 months. After that time period your need for closely monitored PT will depend on your anticipated demand that you will place on the knee.
What if I have more questions?
I encourage you to return to the office for further discussion at any time. You can also contact us.
"*" indicates required fields
Our Location
Dr. Christopher K. Jones, MD
4110 Briargate Parkway #300
Colorado Springs, Colorado 80920
Hours
Monday: 9am-5pm
Thursday 9am-5pm
Friday 9am-5pm
