Frozen shoulder, or adhesive capsulitis, is a relatively common cause of disabling shoulder pain and dysfunction. When a patient comes into my office with severe pain in the shoulder, providing frozen should diagnosis and treatment is always at the top of my list as I begin to evaluate their case. Although it is not as common as a rotator cuff problem, the pain it causes is typically much more severe.
Frozen Shoulder – Symptoms and Causes
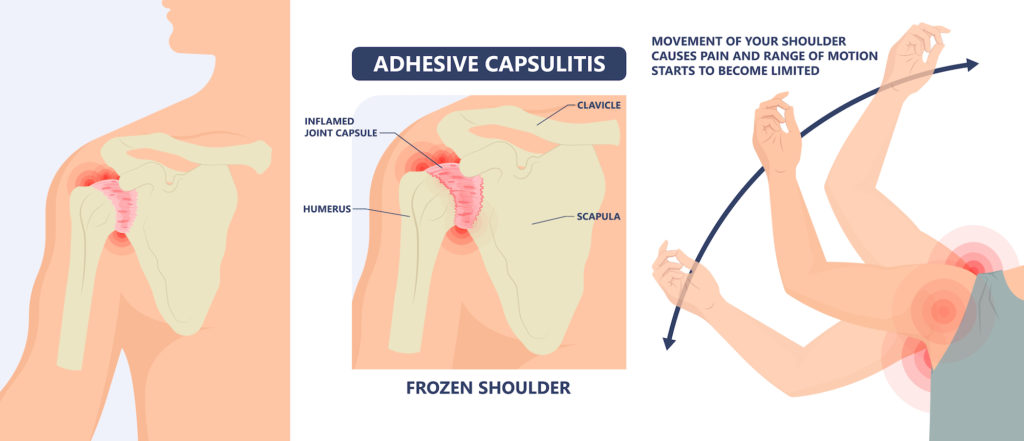
Affecting about 3-5% of the general population, frozen shoulder is not very common. It tends to affect patients between the age of 40 and 60. We don’t yet fully understand the cause of this problem. It typically involves scarring and contracture of the joint capsule. This ends up limiting the mobility of the shoulder joint.
While many of those affected by frozen shoulder do not have any predisposing conditions, it is much more common in patients with diabetes, hypothyroidism or hyperthyroidism, cardiovascular disease, fibrocystic breast disease, and Parkinson’s disease. It can also develop following trauma to the shoulder, or even after shoulder surgery.
Frozen Shoulder – Prognosis and Treatment
The hallmark physical exam finding of frozen shoulder is loss of passive and active mobility of the shoulder joint. Patients often do not realize the significant loss of motion as it usually develops slowly. They subconsciously compensate by using more scapular (shoulder blade) motion.
The good news regarding frozen shoulder is that it will usually get better without any formal treatment. The bad news, however, is that it can take a very long time (up to several years). Patients’ symptoms will often trigger them to seek treatment to shorten the course of this problem.
Conservative treatments include physical therapy for joint mobilizations, oral non-steroidal medications, and steroid injections. These can help improve the pain level and restore functional motion. The primary objective in the treatment of frozen shoulder is to control pain while the problem resolves on its own. Greater than 90% of patients improve with these conservative treatments.
Frozen Shoulder and PRP
Additionally, there have been a few studies that have examined the effectiveness of PRP, platelet rich plasma, in treating this condition. The hypothesis is that the PRP has a direct biologic effect on inhibiting inflammation and promotes healing of the capsule. My experience with utilizing PRP for these patients has been very good. The PRP treated patients typically recover much quicker than those who receive a steroid injection.
Limited studies show growing evidence to support the use of PRP as a therapy for a plethora of orthopedic conditions. It has the benefit of providing a non-operative treatment option for patients when they have run out of other options. Further, there have been no deleterious effects of these injections outside of any other injection. Typically insurance companies do not yet cover PRP treatments–making it an out-of-pocket expense. That, however, is really the only negative aspect.
Other Measures for Frozen Shoulder
Sometimes patients still have pain and functional limitations even after I employ these more conservative measures. At that point, I start to consider surgery or manipulation under anesthesia to restore mobility. Surgery will treat the pain as well.
I perform manipulation under anesthesia with the patient completely sedated by an anesthesiologist with intravenous medication. After the patient is asleep, the surgeon simply manipulates the shoulder in a very specific manner. This manipulation helps to break the scar tissue and restore range of motion. The key to success with this procedure is for the patient to participate in physical therapy. They need to work to maintain the range of motion after I have finished the manipulation.
Is Surgery The Answer?
I consider surgery a last resort, however, I perform the surgery as an outpatient procedure. I typically employ arthroscopy if I determine that surgery is necessary. Arthroscopy involves a minimally invasive approach to the shoulder joint. It uses a camera and special instruments that I insert into the joint via several 1/4” incisions. I utilize the instruments to cut and remove the scar tissue that is restricting movement. This approach is very effective in restoring normal or near-normal range of motion. Patients achieve this affectiveness as long as they do their part and commit to participating in physical therapy.
Following surgery of this kind, we keep the arm out of the sling. I encourage using the full range of motion from the day of surgery. I typically prescribe daily physical therapy for the first couple of weeks after surgery. This helps patients maintain the motion attained during surgery. This procedure is effective in restoring and maintaining the motion of the shoulder in over 90% of the cases that require surgery.
If you believe that you are suffering from a frozen shoulder, contact me. I would be happy to evaluate your shoulder and offer recommendations for treatment.
Please call my office at (719) 822-6277 to request an appointment.





