Meniscal Root Tears
What are they and why are they important?
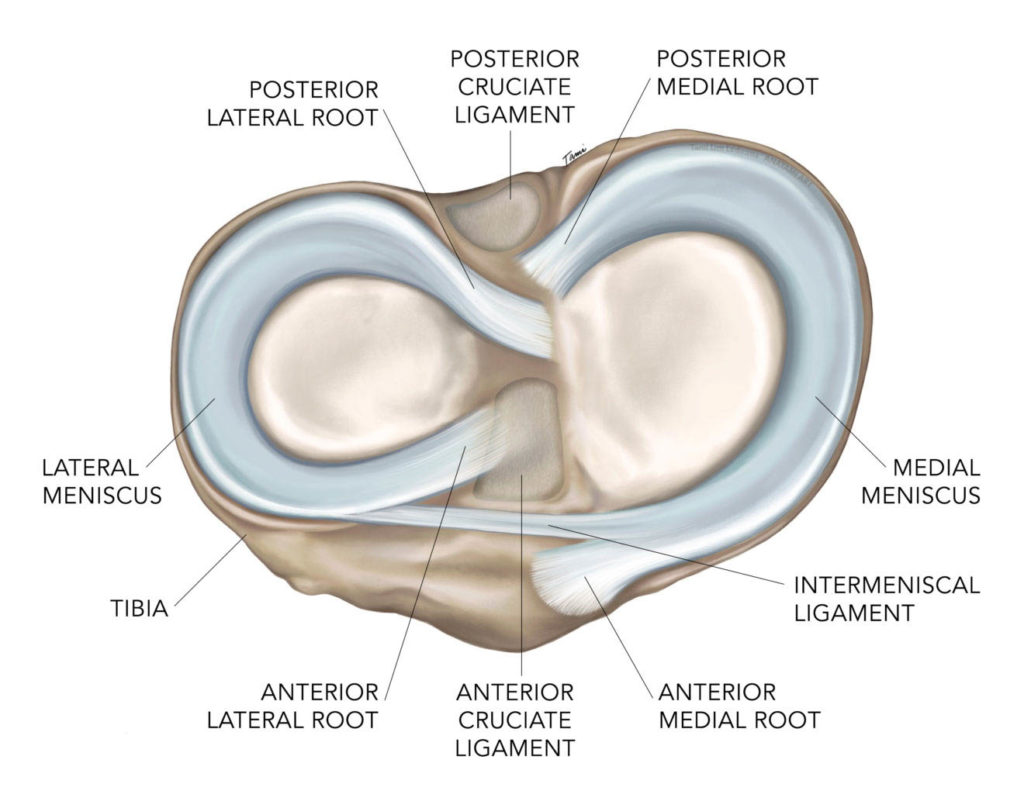
The meniscus is a specialized cartilage structure within the knee joint that serves as a load sharing structure and spreads the contact forces through the knee over a greater surface area. By doing this, less force is seen at any particular point in the knee. The meniscus is a semi-circular structure that by being anchored at each end to the tibia, acts as a ring. These anchors are called “ROOTS”.
The knee joint is composed of the distal femur and proximal tibia, or tibial plateau. The femur has a curved shape, while the tibial plateau is convex or flat. Because of this arrangement (curved or spherical structure placed onto a flat surface), the contact forces are focused over a very small area of the tibial plateau. One analogy that I use in describing this to patients is to imagine a bowling ball sitting on a tile floor. The ball may be 12 inches in diameter, but only 1/4” of its surface is in contact with the floor, so the entire weight of this ball will be focused on this very small area.
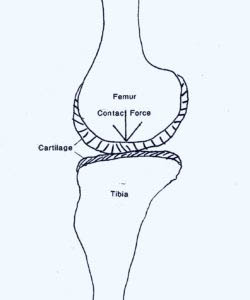
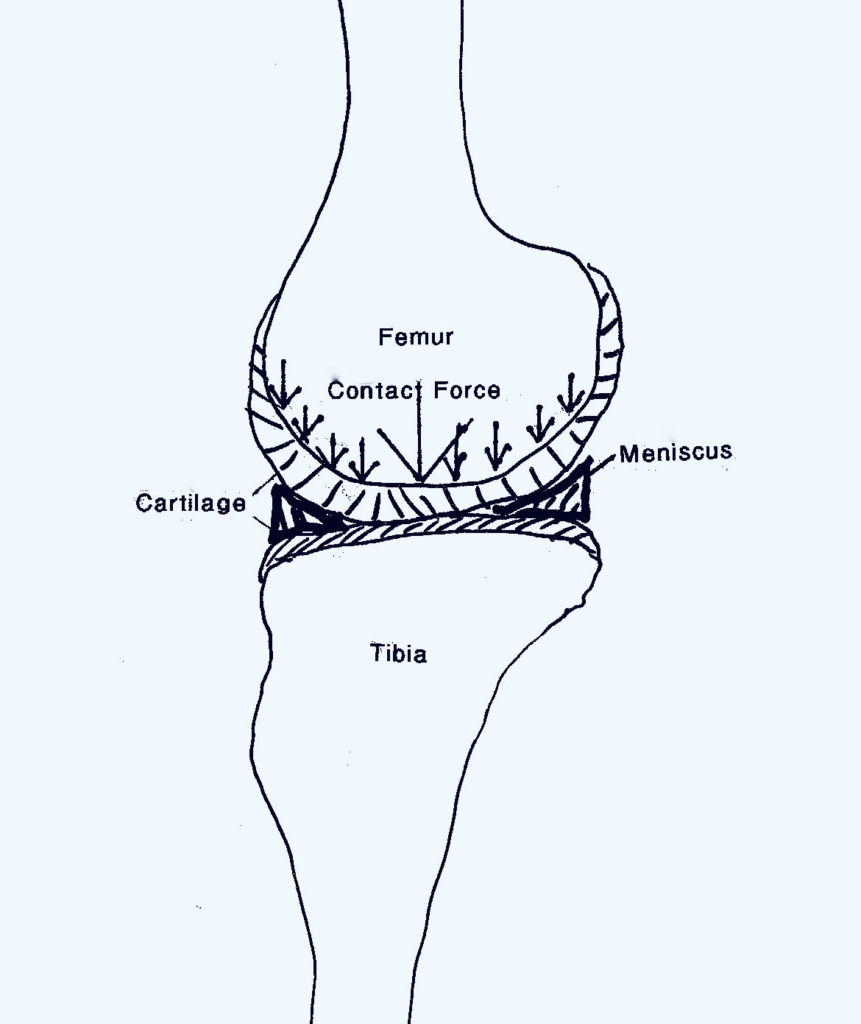

The meniscus sits between the femur and tibial plateau and cradles the femur. This would be similar to a ball sitting on top of a ring that is smaller than the ball. The ball simply sits up on top of the ring. However, if this ring is disrupted, the ball will fall through the ring and put the entire force of the ball on the surface below.
Mechanism of Injury and Symptoms
Root tears typically result from a traumatic event. This can occur with a hyper flexion injury. It can also result from a direct impact to an extended knee. I have seen these injuries occur when someone misses a step and comes down onto an extended knee on the next step below. Patients will often report hearing or feeling a “pop” when the injury occurs. Some patients come in for evaluation immediately following the injury, while others do not seek care until months later. These patients typically report increasing pain in the medial or lateral joint. This pain is most often described as achy or sore pain, particularly after weight-bearing activity.
Consequences of Injury
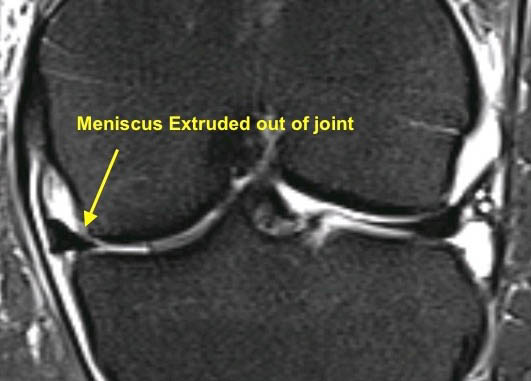
Meniscus root injuries were first described by Pagnani in 1991 and many others have performed biomechanical studies to determine the effects of root tears. When a root tear occurs, the meniscus is extruded (or squeezed) out of the joint. Therefore, it no longer performs its function as a load-sharing structure and all of the force is directed from the femur to the tibial plateau cartilage leading to more accelerated deterioration of the joint. The consequences of this happening are much more severe in cases of lateral meniscus tears. The lateral meniscus is responsible for transmitting 70% of the load in the lateral compartment, whereas the medial meniscus is responsible for only 50% of load sharing. Further, not all people are affected the same. Some patient’s cartilage is more resilient than others and tolerates the increased forces better than others.
Evaluation
As with all injuries, the evaluation begins with taking a history from the patient. Many patients remember a specific event where they felt a pop and subsequently developed increasing knee pain at the joint line. Unlike other meniscal tears where patients report mechanical symptoms (sharp pain that makes the knee give out), these patients typically report achey pain, stiffness and often swelling.
Radiographic evaluation always begins with a good set of orthopaedic X-rays of the knee. This includes weight bearing views in both extension and flexion. These X-rays are evaluated for loss of “joint space” which would indicate loss of cartilage. In patients with advanced arthritis, an MRI is not useful as arthroscopy is not indicated and I focus on treating the symptoms of arthritis using conservative measures such as anti-inflammatory medications, injections, physical therapy and bracing.
If the X-rays show maintenance of joint space, an MRI is ordered to evaluate for acute meniscal or chondral injury. MRIs are very good at identifying meniscus root injuries. The tear is typically demonstrated on the coronal sequences of MRI. Other findings that are characteristic of root injuries include meniscus extrusion and often bone edema, which indicates increased forces are being transmitted to the subchondral bone.

Treatment Options
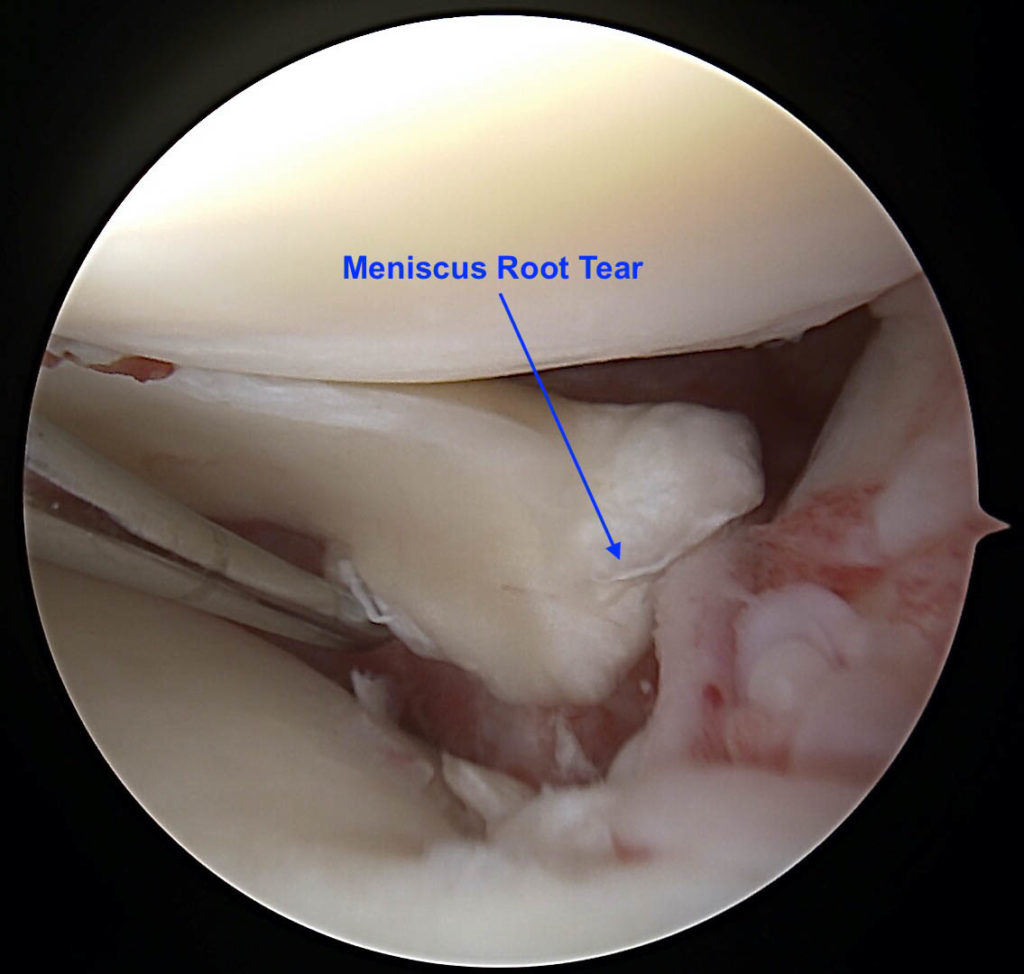
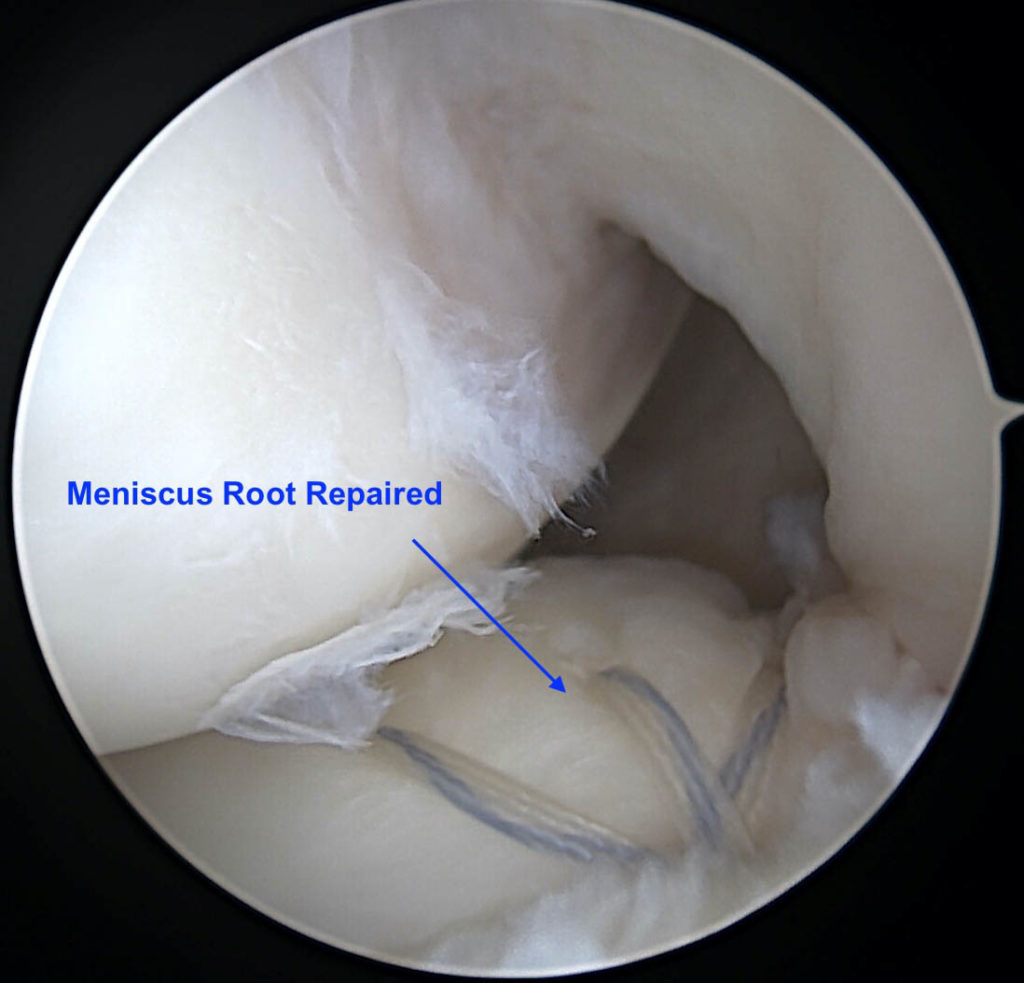
If these tears are identified acutely, the meniscus root is often repairable. Repairing the root will restore the load sharing function of the meniscus and can prevent the rapid destruction of articular cartilage. Root repairs are performed arthroscopically by suturing the meniscus root to its native attachment site. This procedure involves passing sutures through the meniscus and passing these sutures through the tibia. The sutures are then secured to the tibial cortex over a button or by using an anchor.
Arthroscopic Image of Root Tear
Arthroscopic Image of Root Repaired
Post Operative Protocol
After repairing the meniscus root, it is imperative that the patient remain 100% non-weight bearing for 6 weeks. Following this 6 weeks, they begin weight bearing at 25% with crutches for 1 week, and then 75% weight bearing using 1 crutch for 1 additional week. Next, they begin full weight bearing, but avoid high impact activities for 3 months. If patients put weight on the knee immediately after the repair, the forces on the repair will result in failure as the meniscus will be extruded and the sutures will tear out of the tissue resulting in failure of repair.
Outcomes
When root repairs are successful, this is considered a huge “save” as it can restore the function of the meniscus and prevent the rapid deterioration of the joint. Success rates for meniscal root repairs are difficult to assess as there is not good data in the medical literature. However, it can be said that they are more likely to be successful when they are diagnosed acutely, patients are not overweight and they are able to follow the post-operative protocol and remain non-weight bearing.
Dr. Jones is a fellowship trained Orthopaedic Shoulder and Sports Medicine surgeon who is board certified and has the certificate of added qualification in Orthopaedic Sports Medicine. His practice focuses on arthroscopic treatment of shoulder, knee and elbow injuries. Additionally, he is an expert in Total Shoulder Replacement and participates in the education of surgeons from around the globe and product development in Total Shoulder Replacement and arthroscopic procedures.
If you would like to schedule a consultation with Dr. Jones, please call (719) 822-6277.




