
Rotator Cuff Tears
Rotator Cuff Tears – What you need to Know
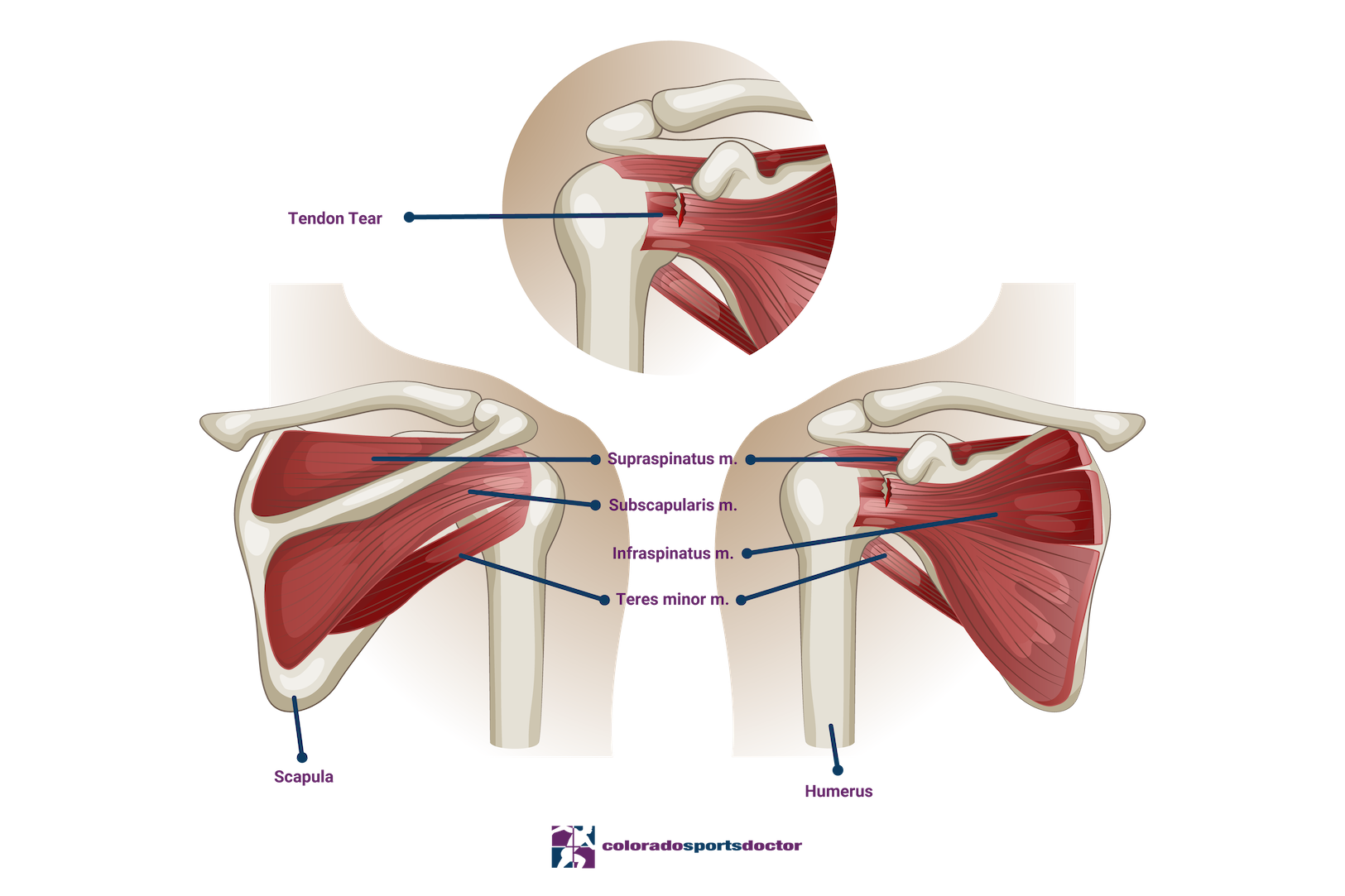
The rotator cuff is a commonly injured group of muscles with varying degrees of strain and tears. The supraspinatus muscle stabilizes and lifts the arm, the Infraspinatus rotates the arm laterally, the teres minor rotates the arm laterally and helps stabilize the shoulder joint, and the subscapularis muscle aids in the internal rotation of the shoulder.
The biceps tendon attaches to the top of the glenoid and passes through the rotator cuff muscles, providing stabilization and support to your shoulder joint. Injuries can occur due to degeneration due to age or overuse of the shoulder or due to an acute traumatic event.
Injuries to the rotator cuff can occur due to the repetitive use of the shoulder joint over time or due to sudden trauma or other factors like a fall, car accident, or sports injury. Rotator cuff tears can be classified as partial-thickness, where the damage does not extend through the entire tendon, or full-thickness, which affects the whole thickness of the tendon. Symptoms of a rotator cuff tear include pain, weakness, and limited shoulder range of motion.
Treatments
Conservative treatment methods for rotator cuff tears include rest, anti-inflammatory medications, and physical therapy to regain strength and range of motion. For partial tears, corticosteroid injections may provide relief.
However, in cases where conservative treatment does not work, surgery may be required to repair the tear. Dr. Jones, a top surgeon, has extensive experience in treating rotator cuff tears using the latest techniques in arthroscopic surgery.
Calcific Tendonitis of Rotator Cuff
Calcific tendonitis refers to a build-up of calcium crystals in soft tissues, and results in a “deposit” that is usually visible on a plain X-ray. The cause of this problem is not well understood, but is known to occur most commonly in the shoulder and is also seen in wrist, elbow, knee, hips and feet. This problem is typically seen in patients between the ages of 30-50 and is more common in women.
The calcium build up can have the consistency of chalk or toothpaste and can initiate a very bad inflammatory reaction in the involved joint. This will cause severe pain. When a patient presents with shoulder pain that is rated 10/10 or they have even been to the Emergency Department with intractable pain, Calcific Tendonitis is the first diagnosis that is considered. Further, the lesion can occupy more space than the normal tendon and can lead to impingement of the rotator cuff into the under surface of the acromial process of the shoulder.
The good news is that Calcific Tendonitis is typically self-limiting, meaning that it will eventually resolve on its own. The bad news is that it can take many years for this to happen. So patients will typically require treatment.
Diagnosis
In order to diagnose this problem your doctor will typically perform a physical exam and get some X-rays. The examination will usually reveal some limitations of shoulder motion and significant pain on provocative test. X-rays will clearly demonstrate the calcium deposit within your rotator cuff.
Ultrasound is also very useful to visualize the deposit.
Treatment for Calcific Tendonitis
Treatment of calcific tendonitis always starts with conservative measures which can include the following – Painkillers and anti-inflammatory medications (ie. Ibuprofen, Naproxyn)
Physical Therapy – rotator cuff rehabilitation in order to restore strength and normal function of the shoulder.
Cortisone steroid injections – can reduce inflammation and can be very effective at controlling the severe pain that this problem can cause.
Ultrasound guided Barbotage – under ultrasound guidance the bursae is anesthesized with local anesthetic and the lesion is then pierced multiple times and “washed” with a combination of local anesthetic and cortisone. Some of the crystals are then aspirated out with the syringe. The remaining crystals are resorbed by the body.
Surgical excision – Arthroscopic treatment is required only when the pain is not controlled with more conservative measures. During the arthroscopic treatment, the lesion is incised and the crystals are removed mechanically. Often this requires a rotator cuff repair be performed on the resulting defect in the rotator cuff.
Recovery
Recovery after surgery depends on the extent of the injury and the type of surgery performed. After surgery, patients may experience pain and discomfort, which can be managed with medications and icing. Rehabilitation will involve a gradual progression of exercises and stretching over several weeks to months.
Regular physical therapy sessions will aid in restoring the range of motion and regaining strength in the shoulder. It is crucial to follow the recovery plan provided by your surgeon to avoid re-injury and to ensure a successful recovery. In the case of rotator cuff injury, it is advisable to seek medical attention from expert surgeons such as Dr. Jones, who combines professional knowledge, skills, and compassion to provide the best care to his patients.
Pre-Operative Risks
Anesthetic Complications
Sore throat – During your surgery, the anesthesiologist will administer anesthesia via an endotracheal tube or an LMA ( laryngeal mask airway). Most patients do not have this issue, but if it occurs, it will usually resolve within 24 to 48 hours. You may use an over the count throat spray to help.
Nausea – This can occur as a direct result of the medications that are used during anesthesia. Some patients are more susceptible to this than others. Our anesthesiologists are very sensitive to this and will do everything possible to prevent it. If you have suffered from this in the past, make sure that you discuss it when you meet them prior to surgery.
Shortness of breath – The vast majority of patients undergoing shoulder surgery elect to have an interscalene block (numbs up your entire shoulder and upper extremity). In roughly 3% this can occur secondary to temporary paralysis of the nerve that goes to their diaphragm on the surgical site. This feeling will go away once the block wears off (12-36 hours).
Surgical Risks and Complications
Bleeding – Bleeding excessively during shoulder surgery is quite rare. I have never had to administer blood to a patient during or after a shoulder operation in 15 years of practice. Medications such as anti-inflammatories (Motrin, ibuprofen, Aleve, naproxyn, Relafen, Indocin, Meloxicam) or blood thinners greatly increase your risk of bleeding and can make it impossible to perform arthroscopic surgery as it impairs visibility. Please stop all of these medications 1 week prior to your surgery. If you are prescribed a blood thinner for a medical condition, please speak to your primary care physician or prescribing provider prior to discontinuation. If there are issues with this, please make my team aware.
Infection – This rarely occurs and has been estimated to occur in less than 1% of surgeries performed. The most common type of infection that occurs is a stitch abscess which is the result of your immune system reacting to the dissolvable sutures. These are simply treated with a short course of antibiotics. Deep infections can occur and usually require further surgery in order to resolve.
Nerve Damage – This is also an extremely rare complication of shoulder surgery and particularly in arthroscopic surgery. If it does occur it is almost always temporary and will resolve over a period of time.
Post-Operative Risks
Stiffness – A small percentage of patients develop a condition called frozen shoulder (adhesive capsulitis) following shoulder surgery. The shoulder loses mobility due to excessive scarring. Sticking with your rehabilitation program will minimize this risk. It will usually resolve with time but rarely requires surgery to release the scar tissue.
Failure of the Repair – Despite the best repair and post-operative rehabilitation program, not all rotator cuff repairs will heal. This is usually related to the size and chronicity of the tear with small and more acute tears healing 95% of the time. But it can also be secondary to the patient not following the post-operative program and re-injuring the shoulder. I will adjust the post-op program if I feel that the patient’s tear requires slower rehabilitation.
What is wrong with your shoulder?
Your shoulder pain arises from a tear of your rotator cuff tendons. A tendon is a thick, cord-like structure that connects muscles to bones. The rotator cuff muscles arise from your scapula and connect to the greater tuberosity of your humerus.
How did this problem start?
The majority of rotator cuff tears are not the result of a single traumatic event, although symptoms can be initiated by such an event. These tears occur as the result of many small injuries that accumulate over time. There is an area in the rotator cuff referred to as “the watershed zone”. In this zone, there is no blood flow and thus the healing capacity of the injured tendons is very limited. Therefore, these small injuries accumulate and result in a complete tear.
What is bursitis?
A bursa is a small sac of fluid that lies between the tendons and bones and serves to act as a cushion and allow the tendons to glide without friction. If this bursa is injured, it will become inflamed and create more fluid than normal. The pain results from the bursa being inflamed.
How is the biceps tendon involved?
The long head of the biceps enters the shoulder between the 2 rotator cuff tendons in the front of your shoulder and attaches to the top of the glenoid (socket). It is exceptionally common for patients with a rotator cuff tear to also have damage to this tendon. This can be treated at the same time as your rotator cuff is repaired. It is typically repaired by relocating its attachment further down your arm. This eliminates it as a source of pain and completely preserves the biceps function.
What does Dr. Jones recommend?
Not all rotator cuffs require repair, but they will not heal on their own. However, if it is causing pain and weakness that is not responding to conservative care, it is best to undergo a rotator cuff repair. At the same time, I can address other areas of pathology as well (biceps, bone spurs, labral tears, arthritis, etc.)
Are there other options available?
If your tear is not completely detached, you potentially could be a candidate for conservative care including physical therapy, activity modifications, steroid injections, or possibly even biologic treatments.
What is the surgery like?
The surgery is done arthroscopically. An arthroscope is an instrument about the size of a pencil that has a camera on its tip that can be inserted into the joint in order to visualize the various structures. Three to five 5-8 mm incisions are made to allow me to insert instruments into the joint and repair the injured tissues. Typically, suture anchors are utilized to reattach the tendon to the bone.
Are the tendons always repairable?
The tendons are repairable in the vast majority of cases. In cases where the tendons are not repairable, I usually have some idea before surgery based on information from your preoperative examination and MRI. If this is the case, there are some other options for you. These include a simple debridement (clean up), superior capsule reconstruction, or reverse total shoulder arthroplasty (please see my articles on these procedures).
What will happen if surgery is not performed?
Your pain will often improve with time, but the tear will not heal. Typically, the pain improves because you are modifying the way you do things and avoid stressing the shoulder. The vast majority of rotator cuff tears will get larger over time and can become irreparable as well.
How long will surgery take and where will it be done?
This surgery typically takes between 1 and 2 hours and is done as an outpatient. Where your surgery is performed depends primarily on your insurance. My team will check into this and get all of the appropriate authorizations. You will go home the same day as your surgery.
How successful is this surgery?
This type of surgery is successful more than 90% of the time in terms of having significant improvement in your symptoms and return to functional activities. The smaller tears generally do better than the large and more chronic tears. A successful recovery will depend greatly on your following of post-operative instructions and participating fully in the rehabilitation process.
What are the potential risks or complications of surgery?
Surgery is a complex and delicate process designed to repair damaged structures deep within the human body. Complications can occur, but fortunately are rare. I have performed thousands of these procedures and take every precaution in order to avoid them. But even when all precautions are taken and the surgery is meticulously performed, they can still occur. Certain factors may slightly increase your potential risks such as previous surgeries on the same shoulder or coexisting medical conditions (ie. diabetes, heart or lung problems, cigarette smoking). The most common complications are outlined below.
When can you return to routine activities of daily living?
You will be able to use your hand, wrist, and elbow at waist level as soon as you are comfortable after surgery. It is CRITICAL that you wear your sling for the entire 6 weeks following your surgery in order to protect the repair while it heals. You may remove your sling for physical therapy, showers, or if you are simply sitting. There will be no active motion of the shoulder during these 6 weeks. Your arm must remain at your side and you can simply move the elbow.
When can you return to work?
For most sedentary jobs, I recommend 3 to 7 days off work. All of your restrictions apply and you must wear your sling. For more physical jobs, you may return to light duty with no lifting, pushing, pulling, or carrying more than 1 or 2 pounds for 6 to 8 weeks. Your restriction will be increased to 5 to 10 pounds at 3 months with nothing overhead. Full release generally happens around 6 months.
How is the shoulder rehabilitated?
Although you will do much of your rehabilitation at home, I strongly advise you to see one of our physical therapists on a regular basis throughout your recovery. They will help keep you on track by following my protocols and advising you on a home program.
What if I have more questions?
I encourage you to contact me via email if you have a clinical question about your surgery. If you have questions regarding insurance, scheduling, or other administrative matters, please contact my team.

