
Total Shoulder Replacement
Total Shoulder Replacement Surgery
The shoulder is the third most common joint to undergo replacement surgery. In the United States, approximately 174,000 to 350,000 total shoulder replacement surgeries are performed each year. In comparison, around 1.15 million hip and knee replacements are completed annually. Because shoulder replacements are less common, fewer surgeons perform them regularly. For this reason, Dr. Jones recommends seeking care from someone who specializes in this specific procedure.
You may consider a total shoulder replacement if pain is not well managed with conservative treatments or if movement limitations affect your quality of life. According to Dr. Jones, when performed appropriately, total shoulder replacement can provide meaningful improvements in function and comfort.
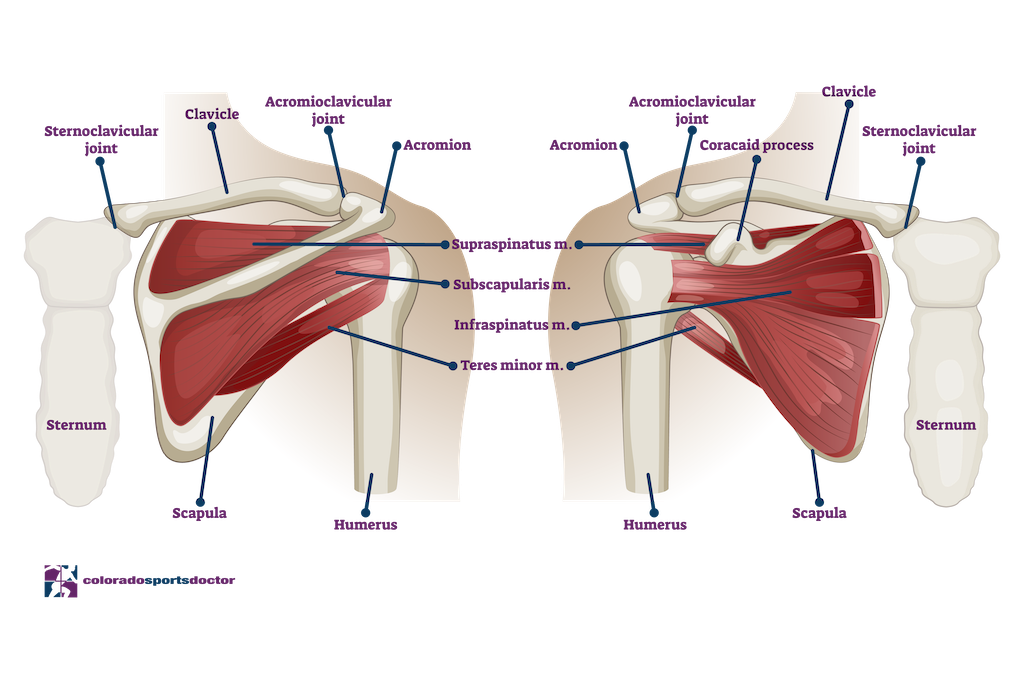
Shoulder Anatomy
The shoulder joint functions as a ball-and-socket joint. However, unlike the hip, the ball is significantly larger than the socket and provides limited natural stability. Dr. Jones often compares the shoulder to “a golf ball on a golf tee.” Because it lacks bony stability, the shoulder relies on a network of ligaments that tighten at specific points to keep the humeral head centered on the socket (glenoid). The rotator cuff muscles also work together to stabilize the joint by balancing opposing forces that center the ball in the socket.
This design allows the shoulder to move with exceptional flexibility. However, it also makes reconstruction or replacement more challenging because of the high levels of pressure and shear forces on the joint. These same forces increase the risk of dislocation or tears. Interestingly, arthritis that requires replacement is less common in the shoulder than in the hip or knee.
Osteoarthritis
Osteoarthritis is a degenerative condition that affects joints with cartilage. As we age, cartilage naturally changes in structure. It develops a higher water content and less collagen, which softens the cartilage and makes it more vulnerable to damage. Over time, cracks or flakes may develop, exposing bone beneath the surface. This bone-on-bone contact often appears on X-rays as a narrowing of the space between the humeral head and glenoid.
As cartilage continues to deteriorate, the joint can become stiff, inflamed, and painful. When conservative care such as physical therapy, anti-inflammatory medication, or activity modification no longer brings relief, Dr. Jones may recommend total shoulder replacement. One of the most common symptoms prompting patients to seek treatment is night pain that interferes with sleep.
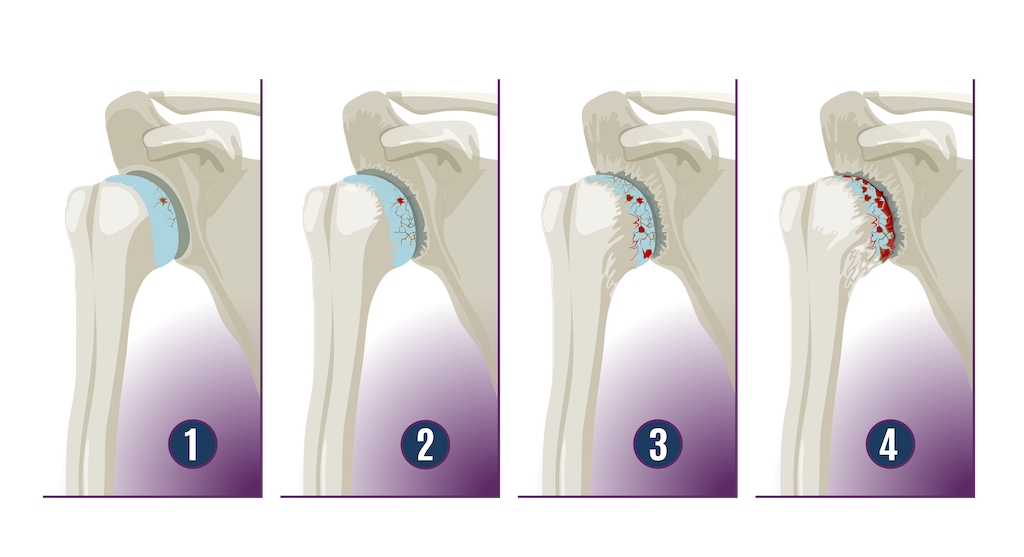
Inflammatory Arthritis
Inflammatory arthritis, such as rheumatoid arthritis, can also damage cartilage. Persistent inflammation breaks down the joint surfaces and leads to bone-on-bone contact. Unlike degenerative arthritis, inflammatory arthritis does not typically cause the bone spurs seen in osteoarthritis. When conservative treatments fail to reduce shoulder pain, Dr. Jones may consider total shoulder replacement to help restore comfort and function.
Avascular Necrosis
Avascular necrosis occurs when part of the bone loses its blood supply, either temporarily or permanently. This may result from conditions such as long-term steroid or alcohol use, injury, rheumatoid arthritis, or an unhealed fracture. Without sufficient blood flow, the affected bone tissue can collapse and distort the joint surface. Although avascular necrosis can occur in any bone, it often affects the ends of long bones like the humerus. When this happens, the shoulder may become painful and movement may decrease.
Proximal Humerus Fractures
The upper arm bone, or proximal humerus, can fracture for various reasons. These injuries are often caused by trauma, such as a fall, and become more common after age 60 when bones may weaken due to osteoporosis. The proximal humerus consists of four parts: the joint surface, greater and lesser tuberosities, and the humeral shaft. When complex fractures occur, these parts can separate into three or four distinct pieces around the ball-and-socket joint.
Fractures of this area can be serious and challenging to repair. Some fractures heal without surgery, while others require fixation using plates and screws. However, Dr. Jones notes that the bone in this region is thin and soft, which can make repair difficult. In such cases, a total shoulder replacement, often a reverse type, may be the preferred approach.
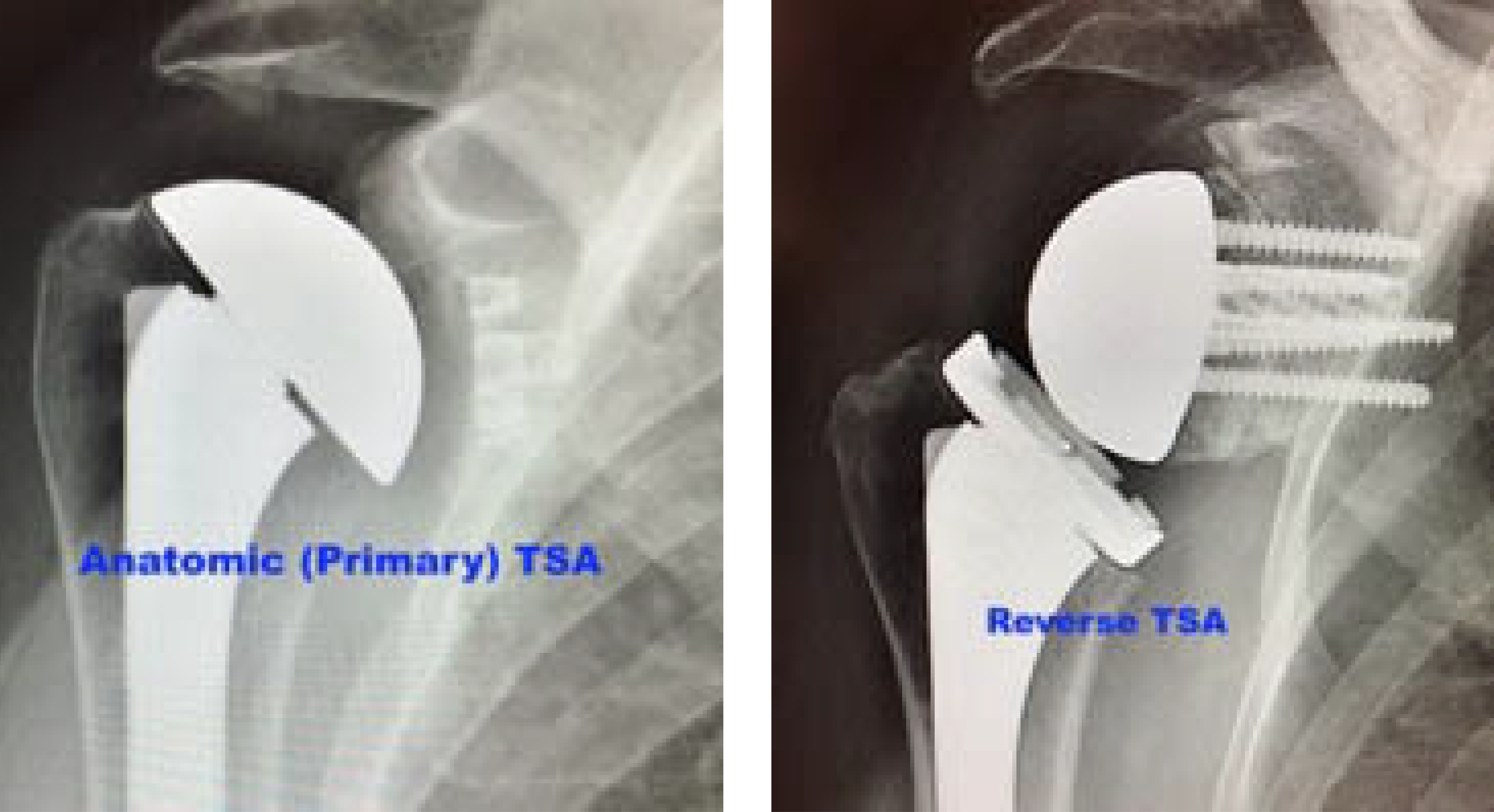
Primary vs. Reverse Total Shoulder Replacement
There are two main types of shoulder replacement procedures: primary (anatomic) and reverse. In a primary total shoulder arthroplasty, the ball and socket are replaced in their natural positions. In a reverse total shoulder arthroplasty, the positions are switched: the ball is placed on the socket side, and the socket is placed on the ball side.
Reverse shoulder replacement is typically performed for patients with long-standing rotator cuff tears or severe dysfunction. Because the rotator cuff no longer stabilizes the shoulder, the reverse design allows other muscles to control movement. Dr. Jones finds this procedure effective for improving mobility when the rotator cuff is no longer functional.
Primary total shoulder replacement is used for patients who still have an intact rotator cuff but suffer from arthritis or cartilage loss. These patients often experience improved movement and less discomfort after surgery, according to Dr. Jones.
Shoulder Treatments
Dr. Jones offers both non-surgical and surgical treatment options for shoulder conditions. Non-surgical treatments may include rest, ice, anti-inflammatory medication, and guided stretching or strengthening exercises. When symptoms persist, patients may be referred to physical therapy or other advanced care options.
If non-operative treatments do not provide sufficient relief, Dr. Jones will review surgical options and recommend the most suitable approach based on each individual’s situation.
Total Shoulder Replacement Surgery Recovery Time
Recovery after surgery requires commitment and careful adherence to post-operative instructions. Dr. Jones provides detailed rehabilitation protocols and works closely with each patient during recovery. Following these guidelines is essential for optimal results.
Many shoulder arthritis patients find that surgical pain is different, and often less intense, than the chronic pain they experienced before surgery. A total shoulder replacement requires additional precautions, as the surgeon must temporarily detach part of the rotator cuff (the subscapularis) to access the joint. Dr. Jones repairs this tendon during surgery, and protecting it during healing is important for long-term shoulder strength and stability.
Most patients notice steady improvement by about three months after surgery. At this stage, many report little to no pain and better function compared to before surgery. Dr. Jones generally advises waiting around three to four months before resuming activities such as golf or other sports.
Join Dr. Jones as he walks you through the steps of Shoulder Replacement Surgery:
"*" indicates required fields
Our Location
Dr. Christopher K. Jones, MD
4110 Briargate Parkway #300
Colorado Springs, Colorado 80920
Hours
Monday: 9am-5pm
Thursday 9am-5pm
Friday 9am-5pm

