
Total Shoulder Replacement
Total Shoulder Replacement Surgery
The shoulder is the 3rd most common joint to undergo replacement surgery. While there are approximately 53,000 total shoulder replacement surgeries performed annually in the US, there are approximately 900,000 hip and knee replacements performed. Because shoulder replacements are relatively uncommon, there are not a lot of surgeons who perform a large number of shoulder replacements. Therefore, it is recommended that you seek out someone who specializes in this procedure.
You should consider a total shoulder replacement if your pain is not controlled with conservative treatments or you have significant functional limitations that are affecting your quality of life. Total shoulder replacement is a wonderful procedure when performed well, and you can expect to have significant relief of pain and improvements in function.
Shoulder Anatomy
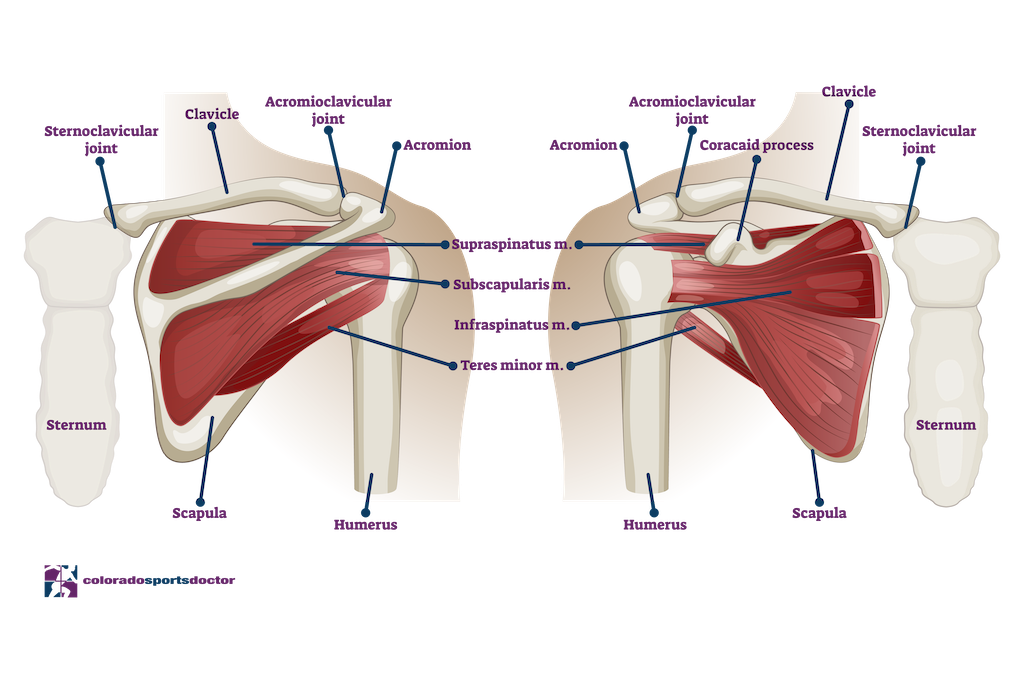
The shoulder joint is considered a ball and socket joint, but unlike the hip, the ball is substantially larger than the socket which offers no inherent stability.An analogy that I often use to describe the shoulder joint is “it is like a golf ball on a golf tee”. Because there is no bony stability, the shoulder relies on a complex arrangement of ligaments that individually tighten at specific limits to maintain the humeral head on the glenoid (socket). Additionally, the rotator cuff musculature offers dynamic stability by synchronously firing opposing muscles to center the ball in the socket.
This complex design allows for an amazing joint with range of motion that is beyond any other joint. This design also makes for a tremendous challenge when trying to reconstruct or replace, as the components are subjected to an enormous amount of compressive and shear forces. It also subjects the shoulder joint to injuries such as dislocation or tears more often than other joints. Interestingly, symptomatic arthritis requiring replacement is not as common in the shoulder as it is in the hip or knee.
Osteoarthritis
Osteoarthritis is a degenerative condition that can affect any joint in our body that has cartilage. Cartilage undergoes changes as we age that can affect its mechanical properties. As we age our cartilage changes to have a higher concentration of water and a lower concentration of collagen ( substance). This results in softening of the cartilage and makes it more prone to damage. As damage occurs, the cartilage can crack or flake off of the bone that it is meant to protect. This can progress to the point that there is exposed bone on the joint surfaces (bone on bone), and can be seen on an X-ray as a loss of “space” between the humeral head and glenoid.
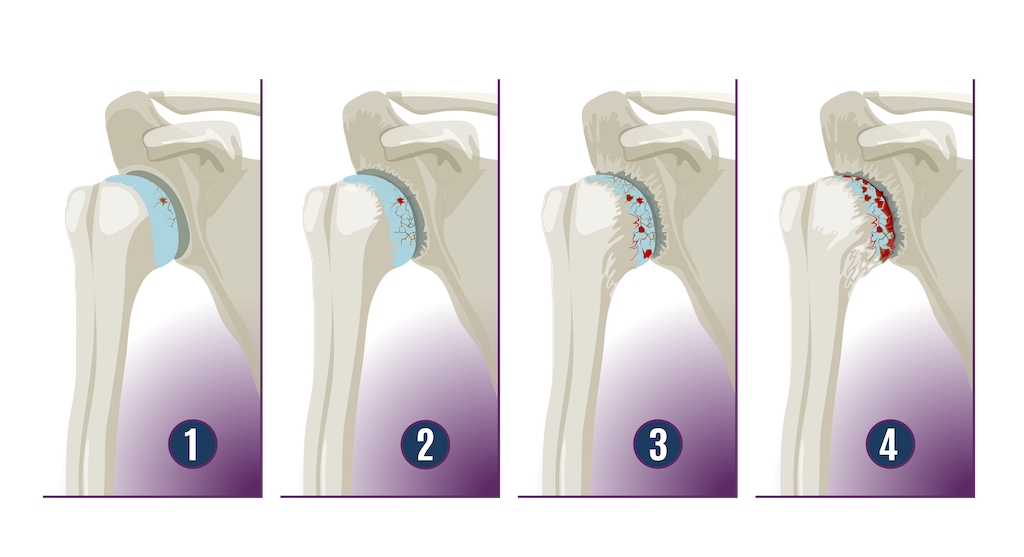
As the cartilage continues to deteriorate the joint will become increasingly stiff, inflamed, and painful. If conservative measures such as physical therapy, anti-inflammatory medication, and activity modifications fail to provide enough relief, total shoulder replacement is the procedure of choice. One prominent symptom that drives patients to act is night pain that interferes with sleep. Night pain is incredibly common for shoulder arthritis.
Inflammatory Arthritis
Other conditions that can result in cartilage destruction include inflammatory arthritis such as rheumatoid arthritis. In this condition, uncontrolled inflammation destroys the cartilage and results in bone on bone in the shoulder joint. Unlike degenerative arthritis, inflammatory arthritis affected shoulders do not develop the bone spurs that we see in degenerative arthritis. When conservative measures fail to provide adequate relief of shoulder pain, total shoulder replacement is performed with great success in terms of relief of pain and improvement in function.
Avascular Necrosis
Avascular necrosis is a disease in which there is a temporary or permanent loss of blood supply to the bone. A number of conditions, including long-term use of steroids or alcohol, a traumatic injury, rheumatoid arthritis or unhealed fractures can cause the blood supply to the bone to be cut off. As the bone dies, it collapses and results in a joint that is not congruous. Although avascular necrosis can happen in any bone, it usually affects the ends of long bones such as the humerus. When this happens, the shoulder becomes painful and movement becomes limited.
Proximal Humerus Fractures
The upper arm can fracture for a variety of reasons. Proximal humerus fractures are typically caused by trauma-related injuries such as a fall but become more common in persons around the average age of 60 as they become more prone to osteoporosis. The proximal humerus includes four parts: the articulating surface, the greater and lesser tuberosity, and the humeral shaft. When complex proximal humerus fractures occur, they tend to break off into three or four parts in consistent patterns around the ball-and-socket joint.
Fractures are the most severe injuries to the upper humerus and can be difficult to treat. These fractures can often be treated without surgery, but severe fractures often require surgery to repair with plates and screws. However, the proximal humerus is often compared to Humpty Dumpty because the bone is very soft with a very thin shell. This can make it very difficult if not impossible to repair. In these circumstances, patients are better treated with a total shoulder replacement, and most often a Reverse Total Shoulder (see below).
Primary vs. Reverse Total Shoulder Replacement
There are 2 types of shoulder replacements that can be performed, primary (anatomic) shoulder replacement or reverse total shoulder replacement. In primary TSA, the ball and socket are replaced as they are present in your natural shoulder. In reverse TSA, the ball is placed on your socket and the socket is placed on your ball side of the joint.
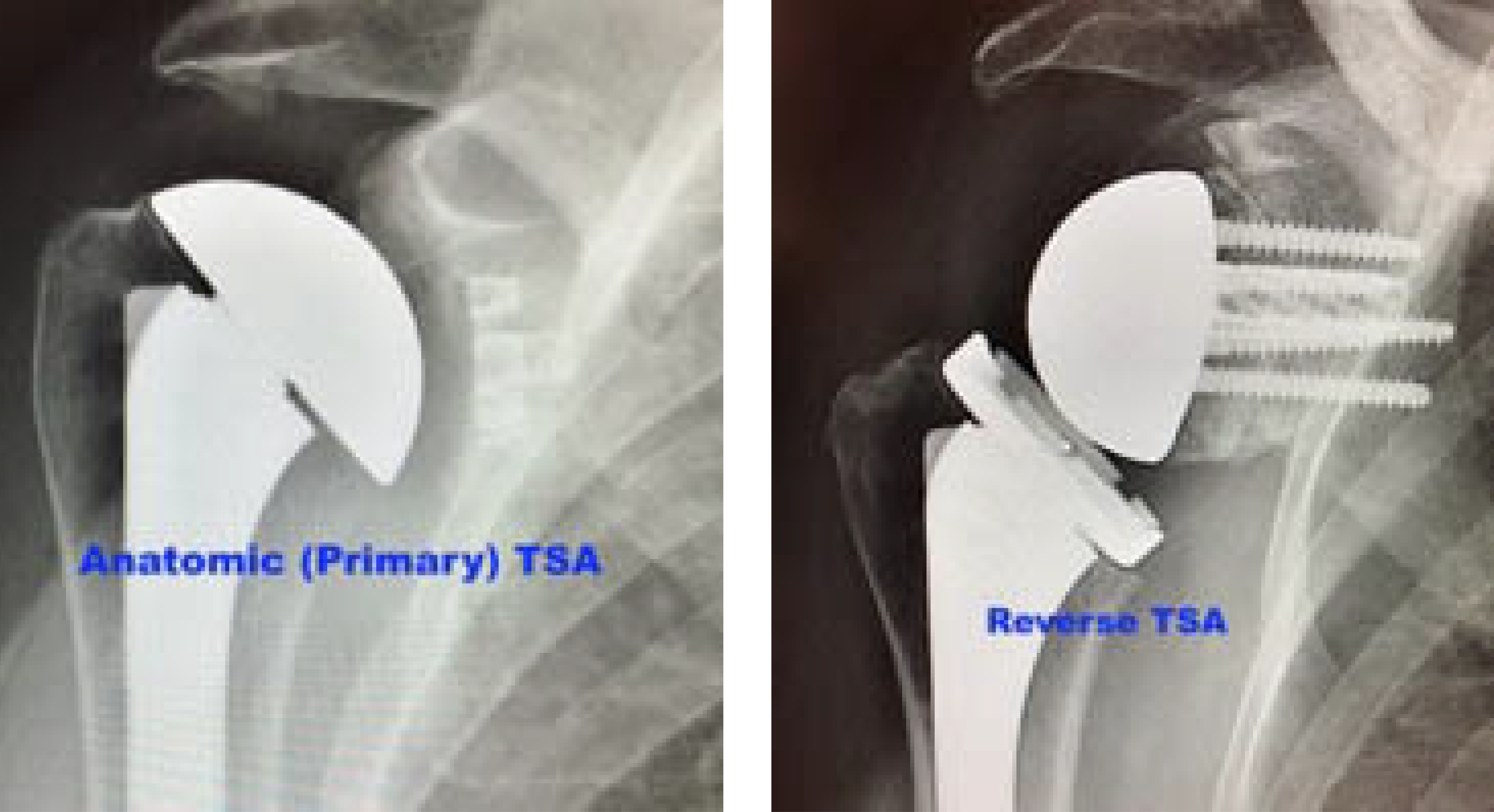
Reverse TSA is performed primarily for patients with rotator cuff deficiency. In these patients, the rotator cuff has been torn for a long period of time and they subsequently develop arthritis or severe shoulder dysfunction because the rotator cuff is no longer performing its job of keeping the ball in the socket. The ball will track properly without the rotator cuff and would result in very poor function with a primary replacement. The reverse is semi-constrained and allows the remaining musculature to move the shoulder without a functioning rotator cuff. This is an amazing procedure and provides tremendous pain relief and improvements in function.
Primary TSA is performed in patients with an intact rotator cuff and degenerative or inflammatory arthritis that has resulted in loss of the cartilage in the shoulder joint. These patients can also expect tremendous improvement in pain and function.
Shoulder Treatments
We offer both non-surgical and surgical treatments that address a variety of shoulder injuries.
Non-surgical treatments often include conservative measures such as rest, use of ice, anti-inflammatory medications, or gentle stretching and strengthening. If needed, patients will be referred to as physical therapy or other methods when severe symptoms do not respond to conservative measures.
If non-operative measures fail, Dr. Jones will discuss your options with you and make the best recommendations based on your personal situation.
Total Shoulder Replacement Surgery Recovery Time
Recovery after any surgical procedure involves a commitment from the patient. They must be willing to accept the precautions/limitations and follow them diligently. I have very specific protocols for each of these procedures and will direct you throughout your recovery. Performing the appropriate rehabilitation is vital in order for you to have your best outcome.
Because shoulder arthritis patients have learned to live with significant pain on a daily basis, the majority of patients report that their pain level after surgery is less than they have been dealing with prior to surgery. They do have “surgical pain” but it is more common for them to state that it is less than they had before undergoing the surgery.
A primary TSA requires a more strict post operative protocol. This is due to the fact that in order to perform the procedure, I have to take a portion of the rotator cuff (subscapularis) off of the humerus to gain access to the joint. At the conclusion of the procedure, I repair the subscapularis and this must be protected so that it heals properly. This is absolutely vital for the best recovery and the long-term survival of your new shoulder.
Most patients are doing really well by 3 months after surgery. They report minimal to no pain and improved function compared to pre-operative status. I typically recommend abstaining from activities such as golf or other sporting activities until approximately 3-4 months after surgery.
Join Dr. Jones as he walks you through the steps of Shoulder Replacement Surgery:
"*" indicates required fields
Our Location
Dr. Christopher K. Jones, MD
4110 Briargate Parkway #300
Colorado Springs, Colorado 80920
Hours
Monday: 9am-5pm
Thursday 9am-5pm
Friday 9am-5pm
