Cartilage is the material that covers the ends of the bones where they contact to become the joint. Articular cartilage is a very durable material that provides a smooth and impact resistant surface and allows the bones to glide over one another during the range of motion.
In the knee, for example, this occurs during activities such as walking, running, and jumping.
Many factors can contribute to cartilage damage, including age-related degeneration of cartilage, excessive weight, repetitive or acute injuries.
During normal activities of life, the cartilage is exposed to extreme pressure. This pressure is increased significantly during activities such as running and jumping. It can be injured from this repetitive stress or from a single traumatic event. The cartilage surface can be sheared off the end of the bone, exposing the underlying bony surface.
Unlike other tissues in our body, injured cartilage does not have the ability to heal as it does not have a blood supply. Without blood, growth factors that initiate healing cannot get to the injured area and initiate a healing response.
Cartilage damage is what ultimately leads to arthritis. This doesn’t mean that everyone who has some cartilage damage has or will ultimately get arthritis, but it is the precursor to the development of an arthritic joint.
It is important to note that cartilage is not created equal in all people. It is evident that some patient’s cartilage is more prone to degenerative changes than others. In fact, it is not uncommon to see patients still in their 30’s or 40’s with advanced cartilage damage without any history of injury. When questioning these patients, there is often a family history of arthritis in their parents and siblings.
How is Cartilage Damage Graded?
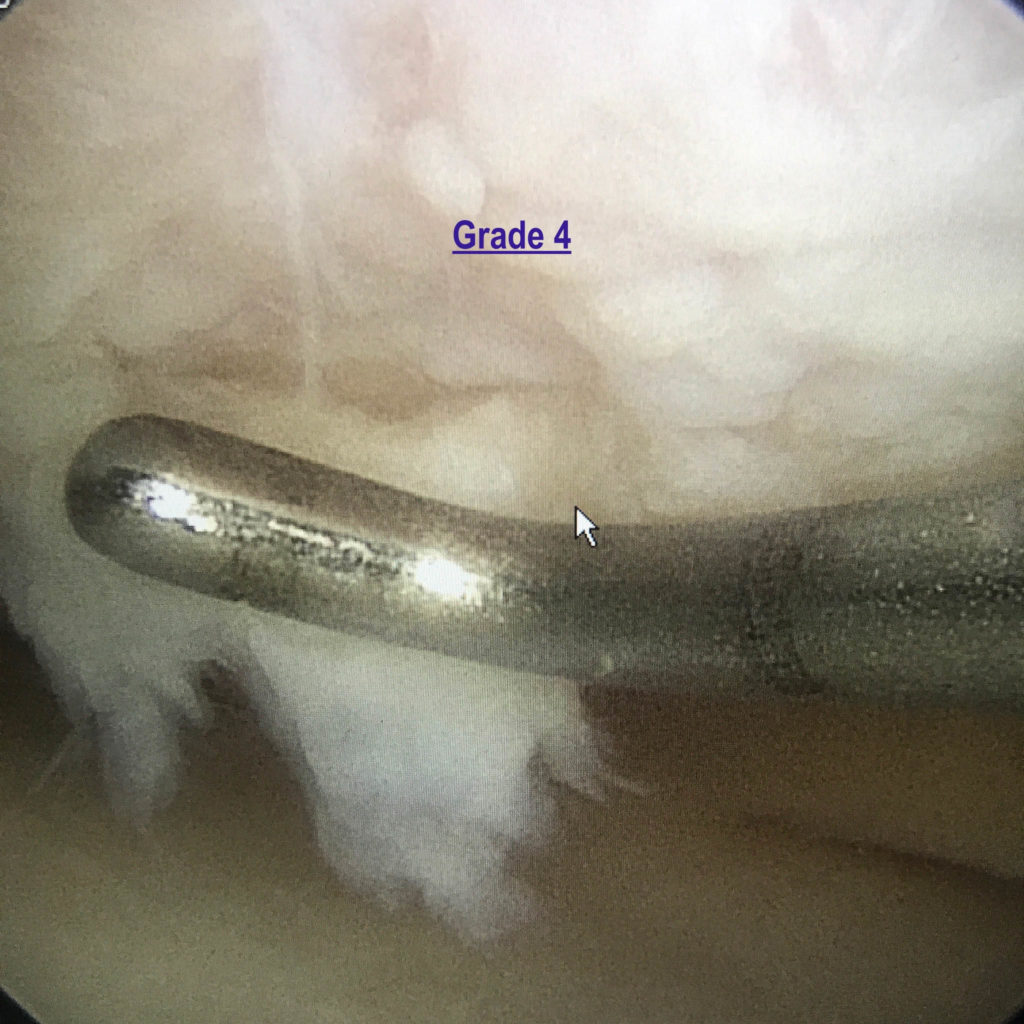
Damaged cartilage is graded from Grade 0 to Grade 4. Grade 0 indicates normal cartilage, with Grade 4 indicating complete loss of cartilage with exposed underlying bone.
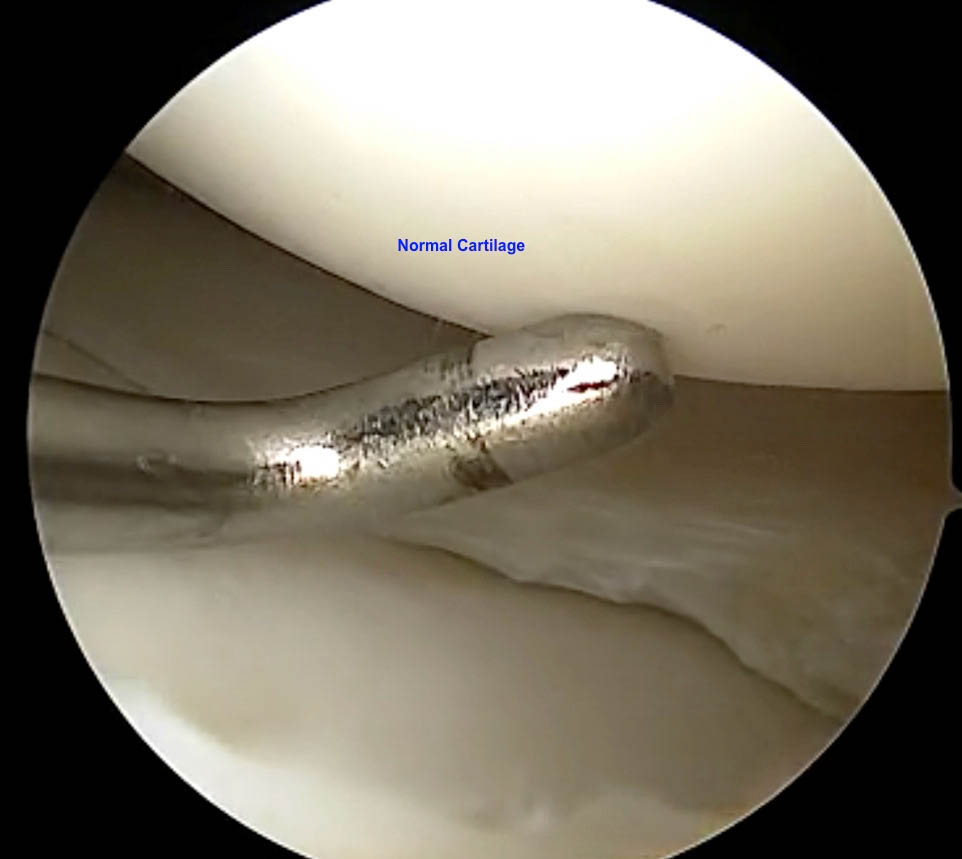
Grade 0 – This indicates normal cartilage with a firm feel to palpation and no surface abnormalities.
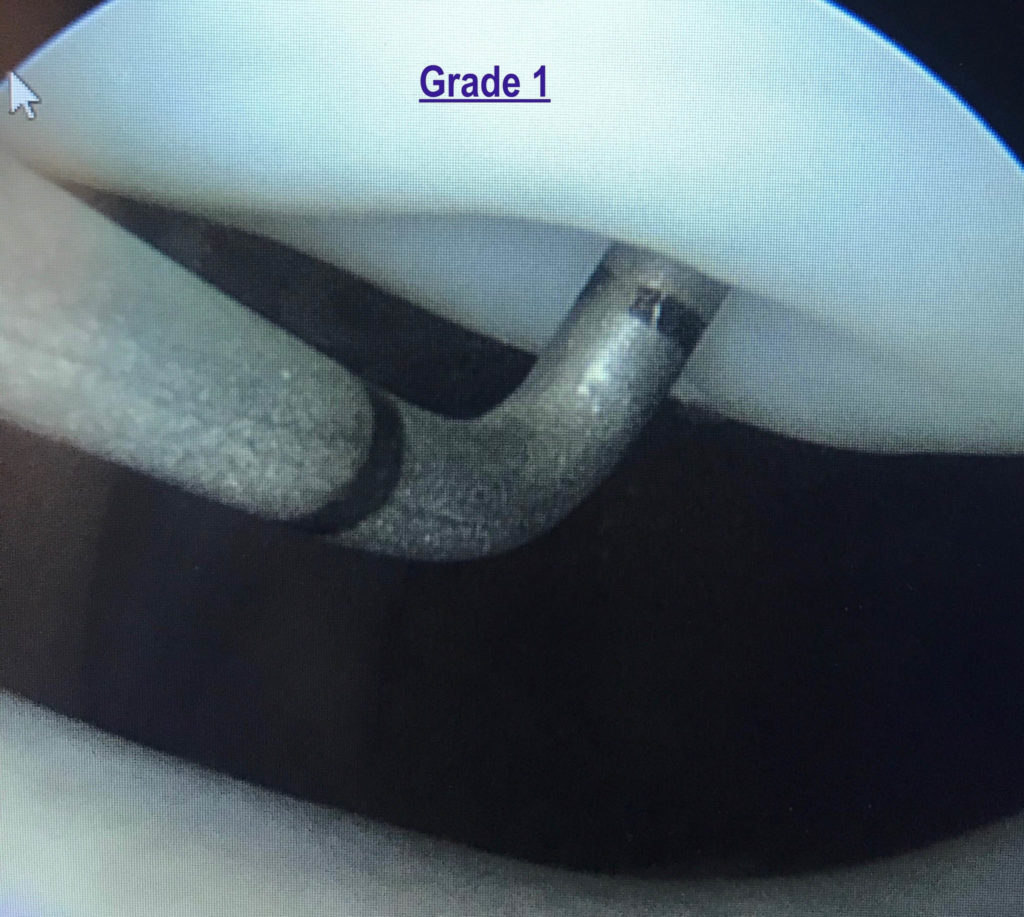
Grade 1 – This involves cartilage that has lost its normal structure and is soft upon palpation. At the time of arthroscopy, this cartilage is easily indented when touched with a probe. Patients with Grade 1 Chondromalacia typically experience pain with intense activity as the cartilage is not protecting the underlying bone as normal cartilage.
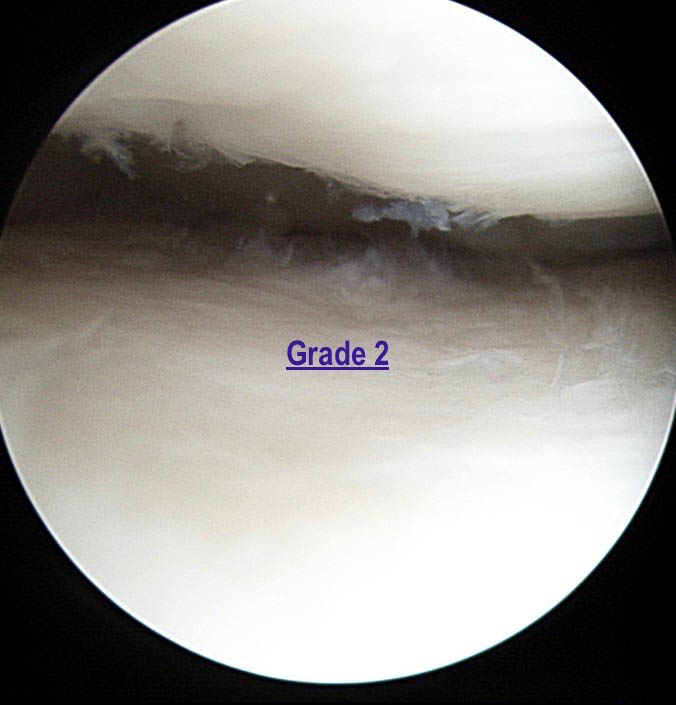
Grade 2 – Grade 2 indicates surface fibrillation or the cartilage having the appearance of shag carpet. These early changes indicate damage to the collagen that forms the structure of cartilage. The collagen fibers that are normally tightly wound, and as the cartilage is damaged, the fibers become unwound.
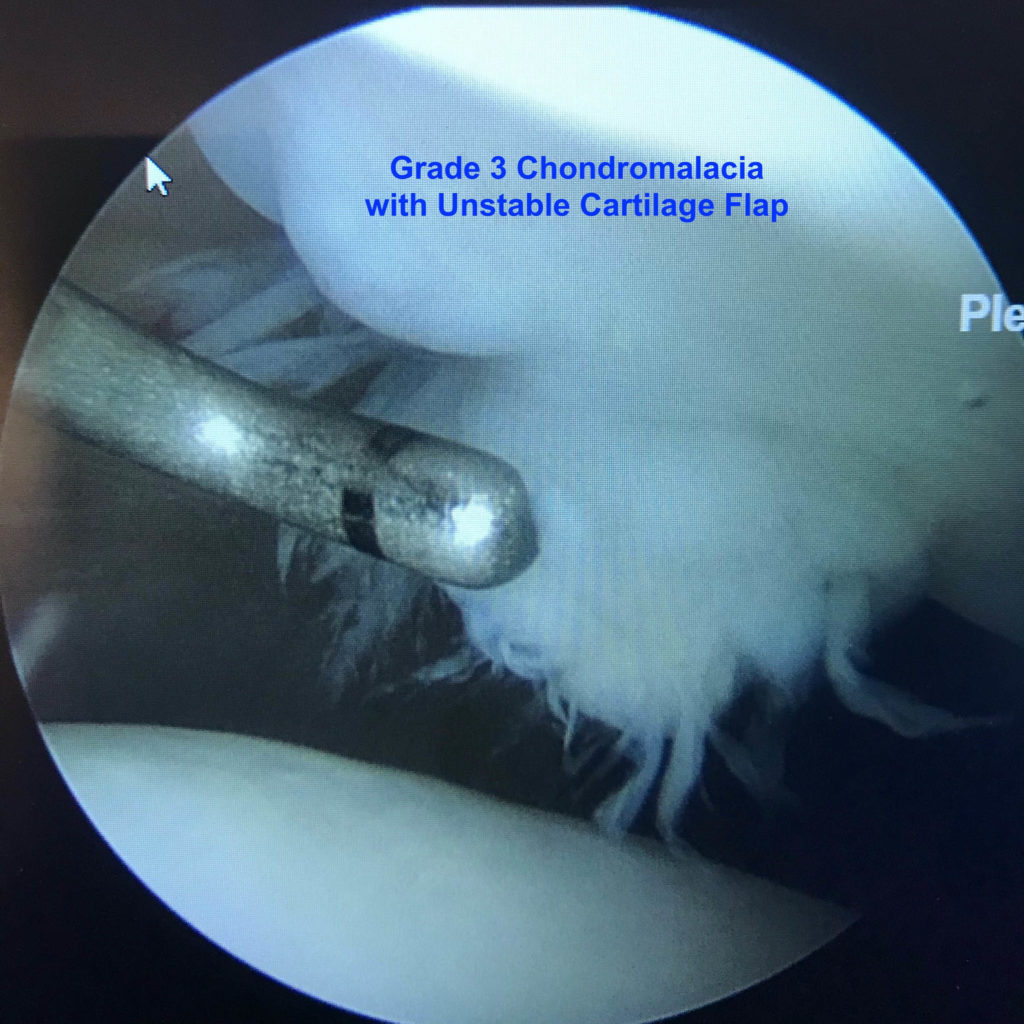
Grade 3 – Cartilage with Grade 3 changes indicate that there is full thickness fissuring or splitting of the cartilage all the way down to subchondral bone.
Grade 4 – Grade 4 chondromalacia indicates that there is complete loss of cartilage with exposed subchondral bone. Grade 4 changes can be focal (involve a small area of cartilage), or it can be diffuse where it affects a large surface area. It can also be monopolar (involve one side of the joint) or bipolar (involves both sides of the joint).
How do you treat Chondromalacia?
The treatment for chondromalacia depends on what type of symptoms the patient is experiencing.
Generally speaking it is best to maintain non-operative treatment unless the patient is experiencing mechanical symptoms (catching or locking), or they have advanced arthritic changes unresponsive to conservative care. If the patient is having mechanical symptoms, it can be quite helpful to perform an arthroscopy to debride or clean up the loose cartilage tissue.
In specific circumstances, they may be a candidate for advanced cartilage reconstruction procedures such as autologous chondrocyte implantation or osteochondral grafts. In patients with advanced arthritis, the best surgical option is either a partial or total knee replacement.
What conservative treatments are available?
Conservative treatments for chondromalacia include activity modification, non-steroidal anti-inflammatory medications (Ibuprofen, Naproxen, Celebrex, Meloxicam, etc.), corticosteroid injections, physical therapy, and maintaining appropriate weight.
Additionally, viscosupplement injections (hyaluronic acid) can be utilized. These injections can help with inflammation and lubricate the joint in order to allow it to move more smoothly. Lastly, there are some relatively new and exciting non-surgical treatment options for chondromalacia referred to as Orthobiologics.
What are Orthobiologics?
Orthobiologics refer to treatments that involve enhancing the patients ability to fight off the inflammation that results from cartilage damage, and in some cases their ability to heal damaged cartilage.
Orthobiologic treatments include the use of the patients’ own blood to create Platelet Rich Plasma (PRP), or their bone marrow to create Bone Marrow Concentrate (BMAC). These products are injected into the involved joint with the goal of adding anti-inflammatory proteins and growth factors to the joint to fight off the inflammation associated with chondromalacia and slowing down the damage to the cartilage.
These Orthobiologics can also be used as a surgical adjunct by injecting them into the joint at the time of arthroscopy in patients with chondromalacia or early arthritis. I have been utilizing these as surgical adjuncts for over 5 years and have seen a dramatic improvement in how much better these patients do after arthroscopy.
You may also see a video that displays the various stages of chondromalacia below.
If you have questions, please feel free to send me an email to:
drjones@coloradosportsdoctor.com




