
Knee Treatments
Knee Anatomy
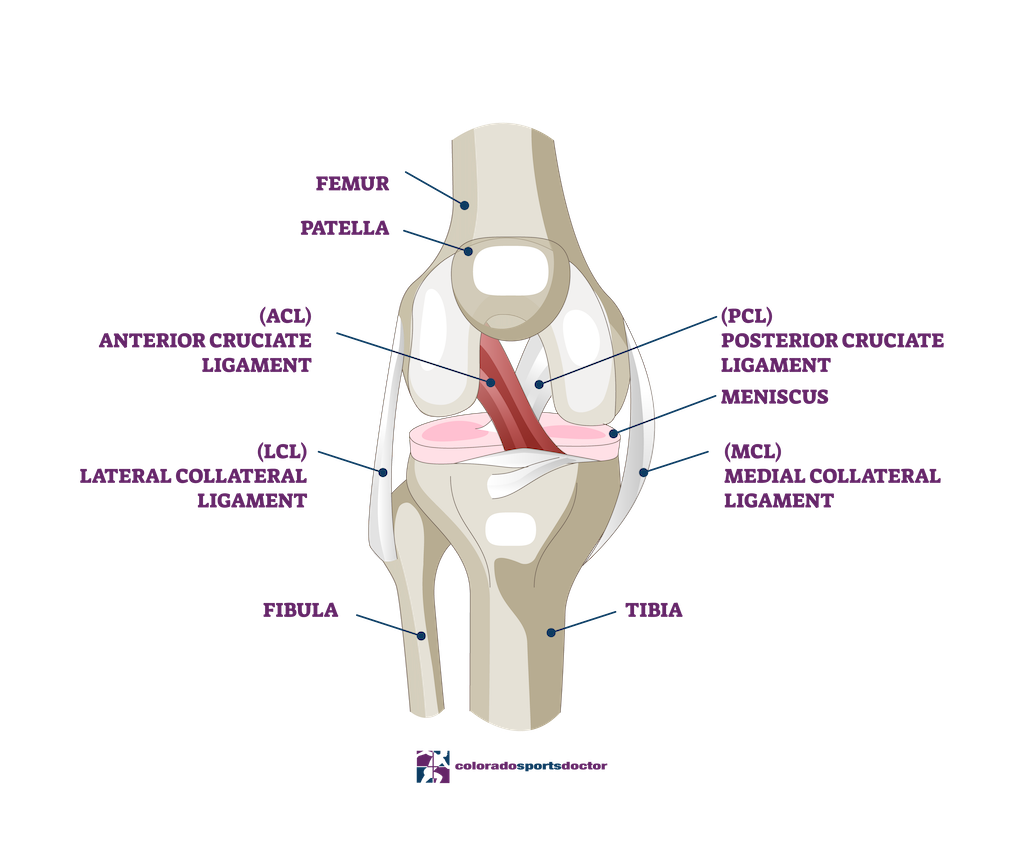
The knee is the largest joint in the body and is a complex hinge joint that connects the thigh bone (femur) to the shin bone (tibia). It also involves the smaller fibula bone in the lower leg. In addition to flexion and extension of the leg, the knee joint also allows for limited rotation and lateral movement. Significant structures surround the joint, including ligaments, tendons, and muscles. The medial and lateral collateral ligaments and the anterior and posterior cruciate ligaments help stabilize the knee joint. At the same time, the quadriceps and hamstring muscles allow for movement of the joint.
The knee joint is covered in hyaline cartilage, which helps to cushion the joint and facilitate smooth movement. The joint also has two shock-absorbing structures called menisci. The synovial membrane lines the joint and produces synovial fluid, which helps to lubricate the joint and reduce friction. Common injuries to the knee joint include ligament sprains and tears, meniscus tears, and patellar dislocations. Treatment for these injuries may include physical therapy, rest, or surgery, depending on the severity of the injury. With proper care and treatment, many knee injuries can be fully recovered, allowing for a full range of motion.
Knee Pain
Is knee pain keeping you from living your life? Dr. Chris Jones offers the latest in non-surgical and surgical treatments for knee pain so you can get back to your life as quickly as possible. He has helped many patients in Colorado Springs recover from their injuries, and he can do the same for you.
Knee Treatments and Specialties
ACL Tears
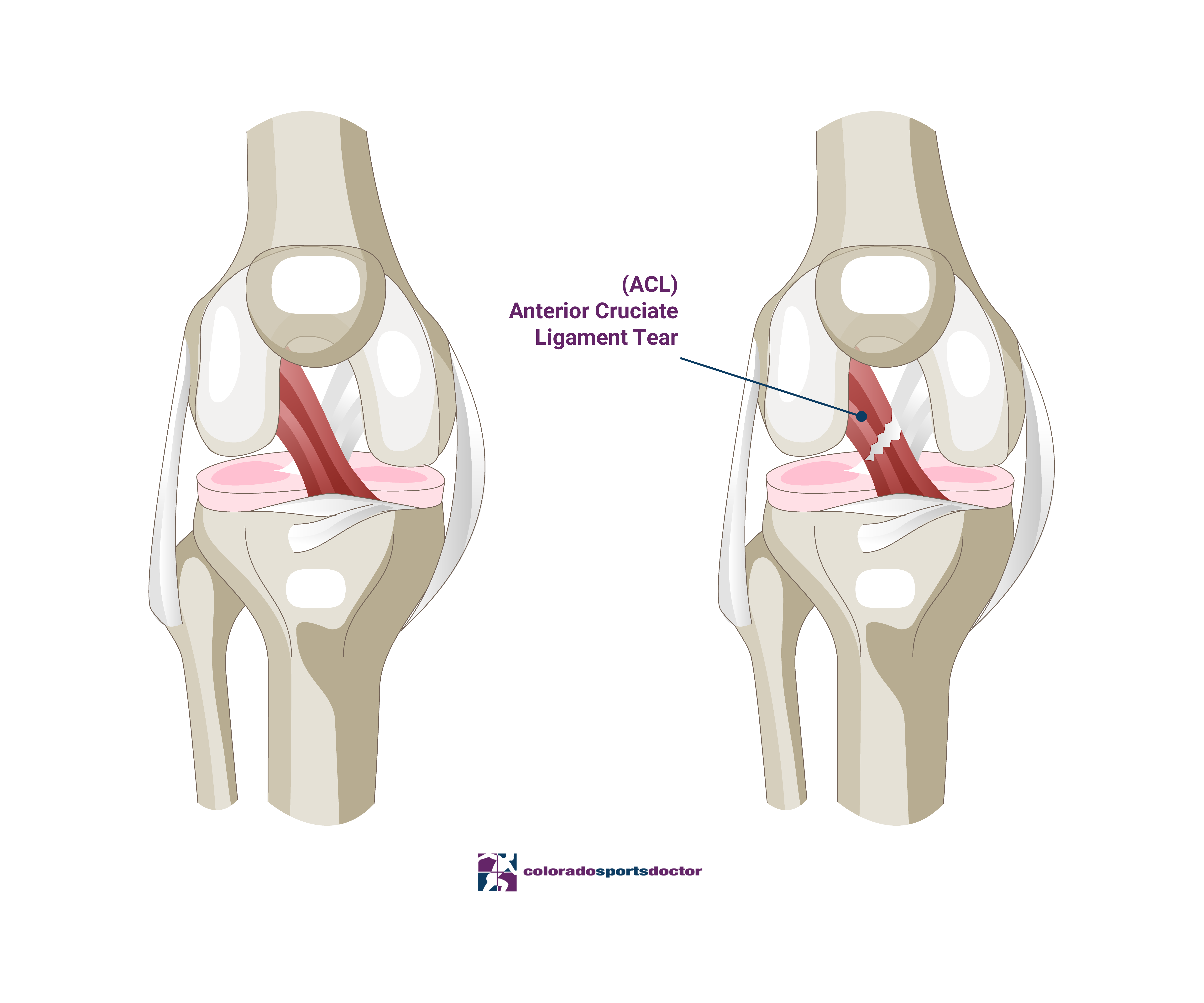
An anterior cruciate ligament (ACL) tear is a common knee injury typically occurring during high-impact sports or activities involving sudden, twisting motions. The ACL is one of the four major ligaments in the knee joint and stabilizes the knee during specific movements, such as pivoting or changing direction. When the ACL is torn, it can cause pain, swelling, and instability in the knee.
Treatment for an ACL tear depends on the severity of the injury and the individual’s activity level. In mild cases, physical therapy and rest may be enough to allow the ligament to heal independently. Surgery may be necessary to repair or reconstruct the torn ligament in more severe cases.
Recovery time varies depending on the extent of the injury and the individual’s rehabilitation progress. With proper treatment and rehabilitation, many people can return to their previous level of activity after an ACL tear.
It’s crucial to properly warm up before physical activity, wear proper athletic shoes, and strengthen the muscles surrounding the knee joint through exercise and physical therapy to prevent ACL tears.
Cartilage Injuries
Cartilage injuries in the knee involve damage to the articular cartilage, the smooth, durable material covering the ends of bones in the joint. This cartilage allows for seamless movement during activities like walking and running. However, age-related degeneration, excessive weight, and repetitive and sudden acute injuries can damage the cartilage. Symptoms of cartilage injuries include pain during weight-bearing, swelling, and sensations of catching, locking, or instability in the knee. Diagnosing these injuries can be challenging due to the variability in symptoms, often requiring diagnostic imaging or direct inspection via arthroscopy.
Treatment for cartilage injuries aims to alleviate pain and restore knee function. Options include chondroplasty to clear out loose cartilage, microfracture to stimulate a healing response, osteochondral autografts and allografts to transplant healthy cartilage, and autologous chondrocyte implantation (ACI) to use the patient’s cultured cells to repair the lesion. Selecting the appropriate treatment depends on the injury’s size, location, and severity to improve joint stability and reduce symptoms.
Meniscus Injuries
The meniscus is a crescent-shaped fibrocartilaginous structure located within the knee joint. In the knee, the medial meniscus is on the inner side, and the lateral meniscus is on the outer side. The meniscus functions to distribute body weight and load throughout the knee joint, as well as to prevent the femur and tibia from rubbing against each other. It also helps shock absorption, lubrication, and knee joint stability.
Meniscus tears are a common knee injury, especially among athletes and older adults. Meniscus tears often occur from sudden twisting or turning movements or a direct blow to the knee. The symptoms of a meniscus tear include pain, swelling, locking or catching of the knee, and difficulty in straightening the knee. Treatment for a meniscus tear may consist of rest, ice, compression, elevation, and physical therapy to restore strength and flexibility to the knee joint. More severe cases may require surgery to repair or remove the damaged meniscus.
Chondromalacia
Chondromalacia is a condition that affects the cartilage on the underside of the patella (knee cap). The patella is a small bone in front of the knee joint, which helps protect the knee and improve its leverage. The cartilage underneath the patella is crucial in preventing friction and allowing the joint to move smoothly. Chondromalacia is caused by the breakdown or softening of this cartilage, resulting in pain and discomfort in the knee joint.
Chondromalacia is more common in young adults and athletes who put repeated stress on their knees, such as runners and jumpers. The symptoms of chondromalacia may include a dull, aching pain in the knee when the joint is bent or straightened, as well as a cracking or popping sound when the knee is moved. Treatment for chondromalacia may include physical therapy to strengthen the muscles around the knee joint, as well as rest, ice, and PRP injections. In severe cases, surgical intervention may be required to remove damaged cartilage or repair the joint.
Cartilage Restoration
Cartilage restoration is a medical procedure to repair damaged cartilage in joints, essential for smooth, pain-free movement. Cartilage damage, often resulting from injury or degenerative conditions like osteoarthritis, can cause pain, swelling, and impaired function. Various methods exist for cartilage restoration, including non-surgical options like MatrixAutologous chondrocyte implantation (MACI), osteochondral allograft (OCA), stem cells, and platelet-rich plasma (PRP). These treatments aim to stimulate the growth of new cartilage and improve joint functionality.
Recovery from cartilage restoration procedures varies depending on the specific treatment and the patient’s condition, but it typically involves a combination of physical therapy and gradual return to activities. While these procedures can significantly reduce pain and enhance joint function, the outcomes depend on factors like the extent of damage and the patient’s adherence to rehabilitation protocols. Advances in medical techniques continue to improve the effectiveness of cartilage restoration.
Platelet Rich Plasma Therapy (PRP)
Platelet-rich plasma (PRP) knee treatments involve using a concentration of a patient’s platelets to accelerate the healing of injured or degenerated tissues, particularly in the knee joint. PRP is derived from a small sample of the patient’s blood, then spun in a centrifuge to separate the different cell types. The serum or plasma and the platelets are collected at the end of this process.
These platelets are rich in granules containing growth factors that help inhibit inflammation and prevent further cartilage damage. This concentrated PRP is then injected into the knee joint to reduce inflammation, alleviate pain, and promote the healing of damaged cartilage and tissues. It’s commonly used for osteoarthritis, ligament injuries, and chronic tendinitis.
The procedure is minimally invasive and typically performed in an outpatient setting, often requiring multiple sessions for optimal results. Recovery times are generally shorter than surgical interventions, with most patients experiencing reduced pain and improved joint function within a few weeks to months. PRP knee treatments involve using a concentration of a patient’s platelets in an effort to accelerate the healing of injured or degenerated tissues, particularly in the knee joint.
Bone Marrow Concentrate Therapy (BMAC)
Biologic treatments like Platelet-Rich Plasma (PRP) and Bone Marrow Concentrate (BMC) are advanced therapies offered by Dr. Jones, a fellowship-trained orthopedic surgeon. Unlike many “stem cell clinics,” Dr. Jones leverages extensive expertise to treat musculoskeletal issues that do not have straightforward surgical solutions. Inspired by European research, he has used these treatments for over a decade to enhance healing in conditions like degenerative tendon injuries, displaying remarkable improvements in patient symptoms and recovery.
These therapies are versatile, serving as standalone treatments or surgical adjuncts for conditions such as medial and lateral epicondylitis, partial rotator cuff tears, knee medial collateral ligament tears, and osteoarthritis. PRP and BMAC help diminish inflammation and promote healing, improving the quality of life and potentially slowing disease progression. Though considered experimental by insurers, making them a direct expense for patients, Dr. Jones strives to offer these cutting-edge treatments affordably while ensuring the best possible outcomes through continuous evaluation and refinement of his protocols.
"*" indicates required fields
Our Location
Dr. Christopher K. Jones, MD
4110 Briargate Parkway #300
Colorado Springs, Colorado 80920
Hours
Monday: 9am-5pm
Thursday 9am-5pm
Friday 9am-5pm
